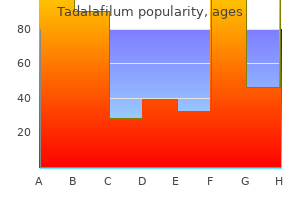
Tadalafilum
Tadalafilum dosages: 20 mg, 10 mg, 5 mg, 2.5 mg
Tadalafilum packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Moderate cholestasis erectile dysfunction at age 23 , with mildly elevated alkaline phosphatase and -glutamyl transpeptidase levels, also can be present, especially in patients with cirrhosis. The annual incidence of hepatocellular carcinoma in patients with chronic hepatitis B varies from 1% in patients without cirrhosis to 2 to 8% in cirrhotic patients, with the higher rates occurring in older patients. The most concerning side effects are neutropenia, thrombocytopenia, anxiety, irritability, depression, and suicidal ideation. Renal impairment and decreases in mineral bone density are rarely seen with tenofovir disoproxil fumarate; these side effects are not observed with tenofovir alafenamide because the active compound is concentrated in the liver. Long-term treatment with nucleoside/nucleotide analogues is indicated in the majority of patients with chronic hepatitis B. Tenofovir (available as tenofovir disoproxil fumarate or tenofovir alafenamide) or entecavir, which are the most potent drugs with an optimal resistance profile, are recommended as first-line monotherapies. In all other cases, treatment should be continued for life and adherence is particularly important. In a patient who develops resistance to any nucleoside/nucleotide analogue other than entecavir or tenofovir, switching to tenofovir (either tenofovir disoproxil fumarate or tenofovir alafenamide) and possibly adding entecavir are the only efficient strategies, although the long-term safety of the combination of tenofovir and entecavir is not known. In patients with lamivudine, telbivudine, or entecavir resistance, treatment should be switched to tenofovir. Patients with multidrug resistance should receive the combination of tenofovir and entecavir. In patients with cirrhosis, nucleoside/nucleotide analogue therapy is the only option. The cumulative incidence of liver decompensation is about 15 to 20% at 5 years in patients with compensated cirrhosis. In patients who are treated with long-term entecavir/tenofovir, however, 8-year survival is now similar to the general population. In addition, the risks of developing cirrhosis, of decompensation of cirrhosis, and of hepatocellular carcinoma are significantly reduced but not eliminated as compared with untreated patients, especially patients who already have cirrhosis or have a family history of hepatocellular carcinoma. The highest prevalence is in Egypt (9% overall, but up to 40% in certain rural areas), where infection was initially spread by intramuscular injections for schistosomiasis during treatment campaigns several decades ago. Rapid diagnostic tests using fingerstick whole blood or saliva, as well as fingerstick whole blood sampled on dried blood spots, can improve access to screening. Laboratory testing often reveals high levels of monoclonal rheumatoid factor and cryoglobulins. This genetic diversity allows continuously generated variant viral populations to be selected by timely changes in the replicative environment. Chronic inflammation triggers fibrogenesis through the activation of hepatic stellate cells. Fibrosis progresses at nonlinear rates that are generally faster in older patients, in males, and in the presence of chronic alcohol intake, viral coinfections, or immunosuppression.
Beebread (Borage). Tadalafilum.
- Atopic dermatitis (eczema).
- Improving growth and development in premature infants.
- What other names is Borage known by?
- Improving the function of the lungs in critically ill patients.
- Dosing considerations for Borage.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96591
Although primary defects of band 3 protein are seen in only about 25% of hereditary spherocytosis patients erectile dysfunction drugs buy , decreased fluorescence intensity is also observed in the erythrocyte membranes of hereditary spherocytosis patients with defects in other membrane proteins such as ankyrin and spectrin. Specialized testing is available for studying difficult cases or cases in which additional information is desired. Useful tests for these purposes include structural and functional studies of erythrocyte membrane proteins, such as protein quantitation, limited tryptic digestion of spectrin, spectrin, and ion transport. Genetic diagnosis of hereditary spherocytosis has become widely available and the associated costs continue to decrease. Next-generation sequencing panels could become a costeffective approach to molecular diagnosis of hereditary hemolytic anemia, especially when the family history is uninformative or when routine laboratory testing fails to identify the causative hemolytic process. Some experts recommend genetic testing to verify the diagnosis prior to splenectomy. Other laboratory manifestations in hereditary spherocytosis are manifestations of ongoing hemolysis. Increased serum bilirubin, increased lactate dehydrogenase, increased urinary and fecal urobilinogen, and decreased serum haptoglobin reflect increased erythrocyte destruction. After diagnosing a patient with hereditary spherocytosis, family members should be examined for presence of the disease. This can be of great epidemiologic importance, particularly for very old and very young patients. Prenatal diagnosis of hereditary spherocytosis has been made in a few cases, but this is rarely necessary. Whether patients with moderate hereditary spherocytosis and compensated, asymptomatic anemia should undergo splenectomy is controversial. This technique results in less postoperative discomfort, a quicker return to preoperative diet and activities, shorter hospitalization, decreased costs, and smaller scars. Even massive spleens can be removed laparoscopically because the spleen is placed in a large bag, diced intraoperatively, and eliminated through suction catheters. Partial splenectomy, initially advocated for infants and young children with significant anemia associated with erythrocyte membrane disorders to allow for palliation of hemolysis and anemia while maintaining some residual splenic immune function, is now being suggested by some for most hereditary spherocytosis patients. Before splenectomy (Chapter 159), patients should be immunized with vaccines against pneumococcus, Haemophilus influenzae type B, and meningococcus. Postsplenectomy care includes counseling of patients or parents to seek prompt medical care in case of febrile illness, prophylaxis if traveling to malaria endemic areas, and importance of seeking medical care after dog or cat bites. Use of routine antibiotics after splenectomy for prevention of pneumococcal sepsis is controversial and data are lacking to indicate or refute their prescription.

Laboratory Evaluation Urinalysis and urine culture should be performed for every patient erectile dysfunction louisville ky . Historically, the four-specimen test was recommended, with specimens obtained from the initial voided bladder urine, midstream voided bladder urine, expressed prostatic secretions obtained during prostate massage, and voided bladder urine collected after prostate massage. Leukocytes without bacteria suggest inflammation consistent with nonbacterial prostatitis. However, this four-step approach is rarely used today because it has not proved to be useful as a diagnostic tool or for directing treatment. In the last week, have you experienced any pain or discomfort in the following areas How often have you had to urinate again less than two hours after you finished urinating, over the last week How often have you had pain or discomfort in any of these areas over the last week How much have your symptoms kept you from doing the kinds of things you would usually do, over the last week If you were to spend the rest of your life with your symptoms just the way they have been during the last week, how would you feel about that How often have you had a sensation of not emptying your bladder completely after you finished urinating, over the last week Antibiotics with good lipid solubility, good enteric bacterial coverage, and a high pKa have the best prostatic penetration. These antibiotics include quinolones, sulfa-based preparations, macrolides, tetracyclines, and aminoglycosides. A13 In cases in which atypical bacteria, such as chlamydia, are suspected to be the cause of chronic bacterial prostatitis, better results may be achieved by macrolide antibiotics, such as azithromycin (500 mg twice daily). Most studies demonstrate effective treatment with 30 days of therapy, but some clinicians prescribe 6 weeks of therapy as for acute prostatitis because the recurrence rate is as high as 40% within a year. Delivery of antibiotics by intraprostatic injection or anal submucosal injection is rarely used today. The optimal regimen for the treatment of chronic prostatitis/chronic pelvic pain syndrome is not known, and the response to treatment is often disappointing. Current empirical therapy uses a combination of -blockers, adrenergic antagonists, phosphodiesterase 5 inhibitors, A15 and anti-inflammatory agents. Neuroleptics, such as gabapentin, have been tried but appear to be no better than placebo and have side effects. Many phytotherapies have been tried, but improvements have not been dramatic or consistent in various trials.

Most defects occur in spectrin impotence natural treatment clary sage , the principal structural protein of the erythrocyte membrane skeleton. Spectrin heterodimers self-associate into tetramers and higher order oligomers that are critical for erythrocyte membrane stability as well as erythrocyte shape and function. Most spectrin defects in hereditary elliptocytosis impair the ability of spectrin dimers to self-associate into tetramers and oligomers, thereby disrupting the membrane skeleton. The precise pathobiology of how elliptocytes are formed in these syndromes is unclear. Genetically, hereditary elliptocytosis is heterogeneous with multiple genetic loci. A wide variety of mutations have been described in the spectrin, spectrin, protein 4. Most cases of hereditary elliptocytosis are inherited in an autosomal dominant pattern, with rare cases of de novo mutations. Splenectomy cures or alleviates anemia in most patients, reducing or eliminating the need for transfusions. After splenectomy, spherocytes remain in the peripheral blood, but their lifespan becomes near normal. In the past, splenectomy was routinely performed in all patients with hereditary spherocytosis. However, the risk of overwhelming postsplenectomy infection; the emergence of penicillin-resistant pneumococci; and the growing recognition of the increased risk of postsplenectomy cardiovascular disease, particularly thrombosis, pulmonary hypertension, and increased risk of atherosclerosis have led to reevaluation of the role of splenectomy in the treatment of hereditary spherocytosis (Chapter 159). In addition, with growing globalization, the important role of the spleen in protection of individuals living in or traveling to geographic regions where parasitic diseases such as malaria or babesiosis occur has reemerged. When splenectomy is considered, health care providers, the patient, and family members must review and weigh the benefits of splenectomy against the immediate and long-term risks of the procedure. Considering the risks and benefits, a reasonable approach is to splenectomize all patients with severe spherocytosis and all patients who have significant signs or symptoms of anemia, including growth failure, skeletal changes, leg ulcers, and extramedullary hematopoietic tumors. The clinical presentation of hereditary elliptocytosis is heterogeneous, ranging from asymptomatic carriers to patients with severe, life-threatening anemia. Most patients with hereditary elliptocytosis are asymptomatic and are diagnosed incidentally during testing for unrelated conditions. Asymptomatic carriers have been identified who possess the same molecular defect as an affected hereditary elliptocytosis relative but who have normal peripheral blood smears. The erythrocyte lifespan, normal in most patients, is decreased in only about 10% of patients.
Ulcerative Colitis Ulcerative Colitis For ulcerative colitis most effective erectile dysfunction pills , colectomy is a curative procedure. Approximately 40% of patients with extensive ulcerative colitis eventually undergo colectomy, usually because their disease has not responded adequately to medical therapy. Emergency colectomy may be required in patients with toxic megacolon or a severe fulminant attack without toxic megacolon. The standard operation for ulcerative colitis is proctocolectomy and a Brooke ileostomy. The most popular alternative operation is total proctocolectomy with an ileal pouch anal anastomosis. In this procedure, a pouch is constructed from the terminal 30 cm of ileum and the distal end of the pouch is pulled through the anal canal. Ileoanal anastomosis is sometimes complicated by inflammation in the ileal pouch (termed pouchitis), which can be treated with antibiotics (typically, metronidazole, 500 mg three times daily or 20 mg/kg/day, or ciprofloxacin, 500 mg twice daily for 2 weeks). When other indications are equivocal, the risk for malignancy (see later) may be an indication for colectomy. Complications Crohn Disease Abscesses Abscesses, which are common complications in Crohn disease, result from extension of a mucosal fissure or ulcer through the intestinal wall and into extraintestinal tissue. Leakage of intestinal contents through a fissure into the peritoneal cavity results in an abscess. Abscesses occur in 15 to 20% of patients with Crohn disease, especially in the terminal ileum. The typical clinical manifestation of an intra-abdominal abscess is fever, abdominal pain, abdominal tenderness, and leukocytosis. Percutaneous drainage of abscesses in patients with Crohn disease may improve the clinical picture but does not provide adequate therapy because of persistent communication between the abscess cavity and the intestinal lumen. Physical examination may reveal postural hypotension, abdominal tenderness over the distribution of the colon, and absent or hypoactive bowel sounds. Agents that reduce gastrointestinal motility, such as antispasmodics and antidiarrheal agents, have the potential to initiate or exacerbate toxic megacolon. Medical therapy is designed to reduce the likelihood of perforation and return the colon to normal motor activity as rapidly as possible. Intravenous fluids should be administered to replete water and electrolyte abnormalities, broad-spectrum antibiotics. Signs of improvement include a decrease in abdominal girth and the return of bowel sounds. Deterioration is marked by the development of rebound tenderness, increasing abdominal girth, and cardiovascular collapse. If the patient does not begin to show signs of clinical improvement during the first 24 to 48 hours of medical therapy, the risk for perforation increases markedly, and surgical colectomy is indicated.

A 40-year-old woman with polycystic kidney disease develops edema and weakness while being prescribed an angiotensin-converting-enzyme inhibitor for hypertension erectile dysfunction and diabetes a study in primary care . She was found to have a serum bicarbonate level of 16 mEq/dL and potassium level of 6 mEq/dL. In the United States, about 640,000 people receive some form of renal replacement therapy each year. A1 However, a larger randomized trial of intensive care unit patients with stage 3 acute kidney injury showed no reduction in mortality, with earlier diuresis in patients who did not receive dialysis. A3 Furthermore, intensive dialytic renal support therapy is no better than standard dialytic therapy, and intermittent hemodialysis and continuous renal replacement therapy lead to similar clinical outcomes in acute renal failure. It also is important to verify that the prescribed dialysis is received and that standardized measures are achieved. Some patients-especially patients in an increased catabolic state, trauma patients, and patients receiving glucocorticoids-may require dialysis more than three times per week to achieve adequate therapy. Neither furosemide nor low-dose dopamine improves outcome, even though low-dose dopamine may temporarily improve metrics of renal physiology. Hemodialysis relies on diffusion across a semipermeable artificial membrane, whereas peritoneal dialysis brings the blood and the dialysate solution in contact across a natural biologic membrane. The diffusion of solutes along their respective concentration gradients across a semipermeable membrane removes nitrogenous waste products and corrects imbalances of potassium, calcium, magnesium, phosphorus, and acid. In addition, plasma water filters across the membrane and, by convection, drags solutes across the membrane in approximately the same concentration as in the plasma water. In the United States, approximately 640,000 patients are currently receiving renal replacement therapy. Hemodialysis involves the flow of blood from the patient to the dialyzer, where diffusion of solutes along their concentration gradient and bulk convection of plasma water across a semipermeable membrane correct many of the acid-base and electrolyte abnormalities in the blood. Renal transplantation, which involves surgically implanting a single kidney from a living or deceased donor, allows more complete correction of these problems and results in improved long-term survival compared with either form of dialysis. However, renal transplantation requires long-term immunosuppressive therapy to prevent rejection, with its attendant increased risk of infection and malignancy. Not all patients are medically suitable for renal transplant, and there remains a substantial shortage of available kidneys (approximately 100,000 patients on the waiting list and only about 20,000 transplants performed annually from about 14,000 deceased donors and about 6,000 live donors). Although short-term success rates of kidney transplant are excellent, long-term results remain disappointing. For example, a typical dialysate solution might use a potassium concentration of 2 mEq/L and a bicarbonate concentration of 35 mEq/L to enable correction of hyperkalemia and uremic metabolic acidosis.
Syndromes
- Greater than 300 mg/dL in adults
- Celiac disease - sprue
- Bronchiectasis (permanent scarring and enlargement of the small sacs in the lungs)
- Other foods that contain no significant amounts of any nutrients
- Decrease in breast size
- Radioactive iodine used for certain medical tests or the treatment of thyroid disease
- MRI or CT scan
- Hematoma (blood accumulating under the skin)
- Therapy to get you to stop drinking (abstinence)
However erectile dysfunction disorder , the conversion rate to an open procedure is about 25% compared with a rate of about 3% for elective laparoscopic surgery. A6 In high-risk patients whose medical conditions preclude cholecystectomy, a percutaneous cholecystostomy can allow prompt gallbladder drainage. A7 If such drainage and appropriate antibiotics do not lead to clear improvement within 24 hours, however, laparotomy is indicated because failure to improve after percutaneous drainage is usually caused by gangrene of the gallbladder or perforation. If cholecystostomy is successful and the acute episode resolves, the patient can electively undergo either cholecystectomy or percutaneous stone extraction and removal of the cholecystostomy tube. Nonsurgical options for the treatment of gallstone disease are rarely used today because of their limited efficacy and the widespread application of laparoscopic cholecystectomy. The direct infusion of organic solvents (methyl tert-butyl ether) into the gallbladder also is efficacious only for cholesterol gallstones, and the recurrence rate is similar to that of oral dissolution therapy. Extracorporeal shock wave lithotripsy can be considered for a single radioopaque stone of any type 0. Inpatient Acute Calculous Cholecystitis Acute Acalculous Cholecystitis Acute acalculous cholecystitis, which accounts for 5 to 10% of all cases of acute cholecystitis, usually occurs in critically ill patients after trauma, burns, long-term parenteral nutrition, and major nonbiliary operations. The cause of acute acalculous cholecystitis remains unclear, although gallbladder stasis with increased bacterial colonization and ischemia have been implicated. The symptoms and signs of acute acalculous cholecystitis are similar to those of acute calculous cholecystitis, with right upper quadrant pain and tenderness, fever, and leukocytosis. The disease often has a more fulminant course than acute calculous cholecystitis and more frequently progresses to gangrene, empyema, or perforation. On cholescintigraphy, the gallbladder does not fill; however, the false-positive rate (absent gallbladder filling without acute acalculous cholecystitis) may be as high as 40%. Emergency cholecystectomy is recommended if the diagnosis is established or even if clinical suspicion is high because the risk for gangrene, perforation, or empyema exceeds 50%. Cholecystectomy rather than cholecystostomy is usually required, but percutaneous cholecystostomy or endoscopic gallbladder stenting is recommended in patients unable to undergo surgery. The mortality rate for acute acalculous cholecystitis can be as high as 40%, mostly because of the concomitant illnesses in patients who develop this disease. Functional Gallbladder Disorder Some patients present with typical symptoms of biliary colic but do not have any evidence of gallstones on ultrasound examination. Some patients may have intermittent gallbladder outlet obstruction due to cystic duct spasm, poor coordination between the contraction of the gallbladder and the sphincter of Oddi, or dysmotility of the gallbladder. An ejection fraction of less than 35% at 20 minutes is considered abnormal, and most of these patients have histopathologic evidence of chronic cholecystitis, although a low gallbladder ejection fraction is not specific for a functional gallbladder disorder (Table 146-2). The efficacy of laparoscopic cholecystectomy is controversial in this setting, but the Society of American Gastrointestinal and Endoscopic Surgeons recommends it. The percentage of patients undergoing cholecystectomy for functional gallbladder disorder in the United States during the past 15 years has increased from less than 5% to more than 20% of patients having the gallbladder removed. Moderate physical activity and dietary management (high fiber intake, avoidance of saturated fatty acids) may lower the risk for gallstone disease.
It measures the time to cessation of bleeding after a standardized incision over the volar aspect of the forearm erectile dysfunction 19 year old male . However, the test is prone to problems related to quality control, reproducibility, sensitivity, and specificity. As an additional replacement for the bleeding time, especially when a functional (qualitative) abnormality of platelets is suspected by characteristic mucocutaneous bleeding or bruising, a global assay of platelet function can be appended to the panel of screening tests. With a few notable exceptions, normal results for all these screening tests of hemostasis essentially exclude any clinically significant systemic coagulopathy. A to C, Algorithms for clinical and laboratory approach to the diagnosis of a patient with a suspected systemic bleeding disorder (coagulopathy). This test provides a global assay of coagulation and fibrinolysis using pointof-care technology. It is a whole blood clotting test in which a small aliquot of blood is rotated in a cuvette, and the strength, elasticity, and dissolution of the forming clot are measured with a torsion wire or by optical detection. A1 Its impact on producing other favorable clinical end points remains open to study. Approach to evaluating patients with prolonged prothrombin time (pt) or activated partial thromboplastin time (aptt). If correction occurs with the inhibitor screen, individual coagulation factor levels should be assayed for a specific deficiency state. Specific assays should then be performed to determine whether there is a true inhibitor against a coagulation factor. These global assays, including thrombin generation tests and viscoelastic assays, have not yet advanced from experimental research to routine clinical practice. These tests measure primarily the coagulation arm of hemostasis and have been shown to be promising in evaluating thrombophilias in guiding antithrombotic therapy. The tests are limited at this time by their lack of validation as a clinical tool. It is crucial to view the clinical setting, history, physical examination, and screening laboratory tests as complementary facets of the approach to patients with suspected coagulopathies. Laboratory testing and possibly further specialized tests of coagulation are indicated for patients whose bleeding histories are suspicious for a hemostatic abnormality. Preoperative screening tests of coagulation are probably warranted for patients who cannot cooperate with an adequate clinical assessment and for those who will be undergoing procedures in which even minimal postoperative hemorrhage could be hazardous. Recent guidelines for preinterventional and preoperative hemostatic evaluation have likewise concluded that bleeding risk requires a detailed personal and family history of hemorrhagic events and physical examination; but individuals with a negative history and without conditions that may interfere with systemic hemostasis should not undergo coagulation testing. Patients usually have deep vein thrombosis of the lower extremities or pulmonary embolism, but other uncommon sites of venous thrombosis may be involved. Arterial thrombosis is not characteristically associated with inherited hypercoagulable states. Arterial thrombosis that occurs prematurely or in the absence of apparent risk factors should trigger a different line of investigation, possibly including evaluation for vasculitis, myeloproliferative neoplasms, hyperhomocysteinemia, antiphospholipid syndrome, and potential sources of systemic embolization.
Evidence of an intrahepatic mass should prompt thorough evaluation for possible malignancy (Chapter 186) erectile dysfunction doctors in tulsa . Biliary obstruction can also occur from malignant diseases, including lymphomatous involvement of the lymphatic tissue in the porta hepatis. Infiltrative diseases, including amyloidosis and granulomatous hepatitis (Chapter 142), should be considered. In the absence of evidence of biliary obstruction or a cause identifiable by noninvasive means, liver biopsy should be strongly considered to complete the evaluation of cholestatic liver test abnormalities. In particular, parenchymal disorders that present with cholestatic liver test abnormalities may mimic biliary obstruction. Because of the risk for life-threatening infection in the setting of unrelieved biliary tract obstruction, this possibility must always be considered and excluded if an alternative diagnosis is not definitely established. A reasonable initial step is the use of a noninvasive imaging study (Chapter 124) such as ultrasonography or magnetic resonance cholangiopancreatography to determine whether the intrahepatic or extrahepatic biliary system, or both are dilated, thereby implying mechanical obstruction. Because of its lesser expense, portability, and convenience, ultrasound is often the procedure of choice, especially if gallstones are suspected. Magnetic resonance cholangiopancreatography may provide more precise resolution, including stricturing of intrahepatic ducts characteristic of primary sclerosing cholangitis. However, each of these techniques can fail to identify dilated ducts, particularly in patients with cirrhosis. Conversely, a modest degree of ductal dilation is common in a patient with a previous cholecystectomy and does not necessarily signify current obstruction. The choice of procedure is based on the suspected site of obstruction (proximal vs. Genetic variations in bilirubin metabolism genes and their association with unconjugated hyperbilirubinemia in adults. Elevated liver enzymes and cardiovascular mortality: a systematic review and dose-response meta-analysis of more than one million participants. These data meant that the fall in plasma bilirubin concentration must have resulted from a decrease in plasma bilirubin turnover, which, in fact, also declined by 75%. Thus, the fall in bilirubin concentration accurately reflected the beneficial effects of steroids on red blood cell survival in this patient with autoimmune hemolysis. She gives a history of episodic jaundice that is most pronounced around times of illness. Measurement of urinary coproporphyrin isomers Answer: E Heritable disorders of bilirubin metabolism should be considered in the setting of a mixed or predominately direct hyperbilirubinemia in the absence of evidence of cholestasis. The diagnosis of Dubin-Johnson syndrome can be established by the measurement of urinary coproporphyrin isomers; the coproporphyrin isomer 1 is generally greater than 80% of total coproporphyrin concentration.
A liver biopsy may demonstrate fibrin-ring granulomas (doughnut shaped) in the background of nonspecific reactive hepatitis and steatosis erectile dysfunction causes and cures . Brucellosis, which is not common in the United States, is caused by at least four species of Brucella: B. The disease is manifested as recurrent high fevers, drenching sweats, malaise, arthralgia, fatigue, abdominal pain, anorexia, and headaches. Hepatic biochemical abnormalities are nonspecific and show elevated serum levels of aminotransferases and alkaline phosphatase. The granulomas formed by this infection are typically smaller than those caused by sarcoidosis or tuberculosis, and a definitive diagnosis can be established by serologic testing. It is important to keep in mind that hepatic granulomas are formed naturally as a consequence of the immune response, so they may be seen in infections with hepatic involvement. Corticosteroids improve liver function test results but do not alleviate portal hypertension, and serial biopsies often show little improvement. Sarcoidosis that leads to portal hypertension and fibrosis may ultimately require liver transplantation (Chapter 145), although sarcoidosis may recur in the new organ. Prospective randomized comparative study of pigtail catheter drainage versus percutaneous needle aspiration in treatment of liver abscess. Percutaneous needle aspiration in uncomplicated amebic liver abscess: a randomized trial. Percutaneous needle aspiration, injection, and re-aspiration with or without benzimidazole coverage for uncomplicated hepatic hydatid cysts. Clinical and epidemiological characteristics of pyogenic liver abscess in people 65 years or older versus people under 65: a retrospective study. Predictors of septic shock in initially stable patients with pyogenic liver abscess. Invasive candida infections in liver transplant recipients: clinical features and risk factors for mortality. Epidemiology and factors associated with amoebic liver abscess in northern Sri Lanka. Infected hepatic echinococcosis: results of surgical treatment of a consecutive series of patients. Biennial versus annual treatment for schistosomiasis and its impact on liver morbidity. Clinical characteristics and outcome of hepatic sarcoidosis: a population-based study 1976-2013. Even this figure is considered an underestimation because milder forms of alcoholic liver disease are not associated with symptoms and often are unrecognized. It has been estimated that alcoholic liver disease accounts for 40% of deaths from cirrhosis and 28% of all deaths from liver disease. It is the second most common indication for liver transplantation in the United States once abstinence from alcohol has been established.
Ines, 41 years: Cystine stones are radiopaque and often form the nidus for secondary calcium oxalate stones.
Murat, 65 years: Consequently, this patient needs to be started on an alternative anticoagulant that is different enough from heparin to not be recognized by the immune response directed against heparin (ruling out answer E).
Kalesch, 27 years: For patients with familial amyloid polyneuropathy, which is an inherited and fatal systemic amyloidosis that is caused by a point mutation in the transthyretin gene, liver transplantation halts the production of the amyloidogenic variant transthyretin, halts the progression of the disease, and significantly improves survival.
Denpok, 44 years: In symptomatic patients and those with impaired renal function, phosphate should be removed by extracorporeal therapy.
Leon, 21 years: Psychogenic purpuras, which are characterized by recurrent focal pain followed by ecchymoses, are controversial and difficult to distinguish from selfinduced or factitious traumatic purpura and bleeding.
Rozhov, 22 years: Validated functional tests for gastroduodenal mucosal perfusion are not widely available, but techniques for directly measuring mucosal oxygen saturation during endoscopy are investigational.
Taklar, 40 years: Silodosin is more effective than tamsulosin for promoting the passage of distal ureteral stones.
10 of 10 - Review by N. Falk
Votes: 87 votes
Total customer reviews: 87