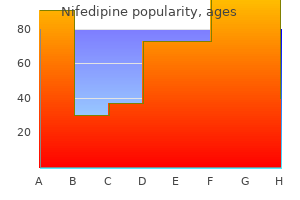
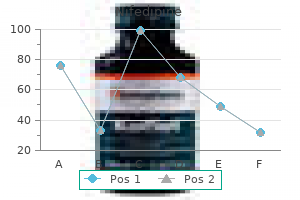
Nifedipine
Nifedipine dosages: 30 mg, 20 mg
Nifedipine packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Cheap nifedipine
It is also performed to irrigate the bladder and to obtain an uncontaminated sample of urine blood pressure for teens buy cheap nifedipine 20 mg on line. When inserting catheters and urethral sounds (slightly conical instruments for exploring and dilating a constricted urethra), the curves of the male urethra must be considered. Just distal to the perineal membrane, the spongy urethra is well covered inferiorly and posteriorly by erectile tissue of the bulb of the penis; however, a short segment of the intermediate part of the urethra is unprotected. Because the urethral wall is thin and the angle that must be negotiated to enter the intermediate part of the spongy urethra, the wall is vulnerable to rupture during the insertion of urethral catheters and sounds. The intermediate part, the least distensible part, runs infero-anteriorly as it passes through the external urethral sphincter. Proximally, the prostatic part takes a slight curve that is concave anteriorly as it traverses the prostate. Urethral stricture may result from external trauma of the penis or infection of the urethra. The spongy urethra will expand enough to permit passage of an instrument approximately 8 mm in diameter. The external urethral orifice is the narrowest and least distensible part of the urethra; hence, an instrument that passes through this opening normally passes through all other parts of the urethra. In persons with large indirect inguinal hernias, for example, the intestine may enter the scrotum, making it as large as a soccer 1506 ball. Similarly, inflammation of the testes (orchitis), associated with mumps, bleeding in the subcutaneous tissue, or chronic lymphatic obstruction (as occurs in the parasitic disease elephantiasis) may produce an enlarged scrotum. Palpation of Testes the soft, pliable skin of the scrotum makes it easy to palpate the testes and the structures related to them. Most health care providers agree that testicular exam should be part of a routine physical exam. Some physicians recommend that men perform a selfexamination of their testicles monthly after puberty and report any testicular or scrotal changes. According to the American Cancer Society, although testicular cancer can occur at any age, about half of all cases occur between the ages of 20 and 34. The lifetime risk of developing testicular cancer is 1 in 263, making it a relatively uncommon type of cancer. Testicular cancer can be treated and usually cured, especially when found early in the course of the disease. Hypospadias Hypospadias is a common congenital anomaly of the penis, occurring in 1 in 300 newborns. In the simplest and most common form, glanular hypospadias, the external urethral orifice is on the ventral aspect of the glans penis. The embryological basis of penile and penoscrotal hypospadias is failure of the urogenital folds to fuse on the ventral surface of the penis, completing the formation of the spongy urethra. It is believed that hypospadias is associated with an inadequate production of androgens by the fetal testes.
Buy nifedipine 30 mg with amex
The presence of a single supernumerary (accessory) tooth is usually seen in the anterior maxilla heart attack alley cheap nifedipine 30 mg buy line. The most common supernumerary tooth is a mesiodens, which is a malformed, peg-like tooth that occurs between the maxillary central incisor teeth. A supernumerary tooth occurs in addition to the normal number but resembles the size, shape, or placement of normal teeth. Multiple supernumerary teeth are rare in individuals with no other associated diseases or syndromes, such as cleft lip or cleft palate or cranial 2143 dysplasia (malformation). The supernumerary teeth can cause problems for the eruption and alignment of normal dentition and are usually surgically extracted. Extraction of Teeth Sometimes, it is not practical to restore a tooth because of extreme tooth destruction. The blow to the tooth disrupts the blood vessels entering and leaving the apical foramen. The lingual nerve is closely related to the medial aspect of the 3rd molar teeth; therefore, caution is taken to avoid injuring this nerve during their extraction. Damage to this nerve results in altered sensation to the ipsilateral side of the tongue. Often, there is not enough room for these molars to erupt, and they become lodged (impacted) under or against the 2nd molar teeth. Dental Implants Following extraction of a tooth, or fracture of a tooth at its neck, a prosthetic crown may be placed on an abutment (metal peg) inserted into a metal socket surgically implanted into the alveolar bone. A procedure to augment the alveolar bone with calf or cadaveric bone may be required before the socket can be implanted. A waiting period of several months may be necessary to allow bone growth around the implanted socket before the abutment and prosthetic crown are mounted. Nasopalatine Block the nasopalatine nerves can be anesthetized by injecting anesthetic into the incisive fossa in the hard palate. Both nerves are anesthetized by the same injection where they emerge through the incisive fossa. The affected tissues are the palatal mucosa, the lingual gingivae and alveolar bone of the six anterior maxillary teeth, and the hard palate. Greater Palatine Block the greater palatine nerve can be anesthetized by injecting anesthetic into the greater palatine foramen. This nerve block anesthetizes all the palatal mucosa and lingual gingivae posterior to the maxillary canine teeth and the underlying bone of the palate. The anesthetic should be injected slowly to prevent stripping of the mucosa from the hard palate.
Diseases
- Chancroid
- Spinal cord injury
- Aerosinusitis
- Verloes David syndrome
- Phenobarbital embryopathy
- Acrodermatitis
- Endomyocardial fibroelastosis
- Frontonasal dysplasia Klippel Feil syndrome
Purchase nifedipine 20 mg on-line
Ischial bursitis is a friction bursitis resulting from excessive friction between the ischial bursae and the ischial tuberosities hypertension jokes trusted 30 mg nifedipine. Localized pain occurs over the bursa, and the pain increases with movement of the gluteus maximus. Hamstring Injuries Hamstring strains (pulled and/or torn hamstrings) are common in individuals who run and/or kick hard. The violent muscular exertion required to excel in these sports may avulse (tear) part of the proximal tendinous attachments of the hamstrings to the ischial tuberosity. Usually, thigh strains are accompanied by contusion (bruising) and tearing of muscle fibers, resulting in rupture of the blood vessels supplying the muscles. Tearing of hamstring fibers is often so painful when the athlete moves or stretches the leg that the person falls and writhes in pain. These injuries often result from inadequate warming up before practice or competition. Avulsion (tearing away) of the ischial tuberosity at the proximal attachment of the biceps femoris and semitendinosus may result from forcible flexion of the hip with the knee extended. When a standing person is asked to lift one foot off the ground and stand on one foot, the gluteus medius and minimus normally contract as soon as the contralateral foot leaves the floor, preventing tipping of 1690 the pelvis to the unsupported side. When a person who has suffered a lesion of the superior gluteal nerve is asked to stand on one leg, the pelvis on the unsupported side descends. Other causes of this sign include fracture of the greater trochanter (the distal attachment of gluteus medius) and dislocation of the hip joint. When the pelvis descends on the unsupported side, the lower limb becomes, in effect, too long and does not clear the ground when the foot is brought forward in the swing phase of walking. To compensate, the individual leans 1691 away from the unsupported side, raising the pelvis to allow adequate room for the foot to clear the ground as it swings forward. Other ways to compensate is to lift the foot higher as it is brought forward, resulting in the so-called steppage gait, or to swing the foot outward (laterally), the so-called swing-out gait. These same gaits are adopted to compensate for the footdrop that results from common fibular nerve paralysis. Paresthesia (nonpainful anesthesia) radiates to the foot because of anesthesia of the plantar nerves, which are terminal branches of the tibial nerve derived from the sciatic nerve. Injury to Sciatic Nerve A pain in the buttocks may result from compression of the sciatic nerve by the piriformis (piriformis syndrome). In approximately 50% of cases, the histories indicate trauma to the buttocks associated with hypertrophy (increase in bulk) and spasm of the piriformis.
Nifedipine 20 mg buy lowest price
Lymphatic drainage of the cecum and appendix passes to lymph nodes in the meso-appendix and to the ileocolic lymph nodes that lie along the ileocolic artery pulse pressure 30 mmhg order genuine nifedipine line. The nerve supply to the cecum and appendix derives from the sympathetic and parasympathetic nerves from the superior mesenteric plexus. The sympathetic nerve fibers originate in the lower thoracic part of the spinal cord, and the parasympathetic nerve fibers derive from the vagus nerves. Afferent nerve fibers from the appendix accompany the sympathetic nerves to the T10 segment of the spinal cord (see also "Summary of Innervation of Abdominal Viscera," p. The colon encircles the small intestine, the ascending colon lying to the right of the small intestine, the transverse colon superior and/or anterior to it, the descending colon to the left of it, and the sigmoid colon inferior to it. It passes superiorly on the right side of the abdominal cavity from the cecum to the right lobe of the liver, where it turns to the left at the right colic flexure (hepatic flexure). This flexure lies deep to the 9th and 10th ribs and is overlapped by the inferior part of the liver. The ascending colon is narrower than the cecum and is secondarily retroperitoneal along the right side of the posterior abdominal wall. The ascending colon is usually covered by peritoneum anteriorly and on its sides; however, in approximately 25% of people, it has a short mesentery. The ascending colon is separated from the anterolateral abdominal wall by the greater omentum. A deep vertical groove lined with parietal peritoneum, the right paracolic gutter, lies between the lateral aspect of the ascending colon and the adjacent abdominal wall. These arteries anastomose with each other and with the right branch of the middle colic artery, the first of a series of anastomotic arcades that is continued by the left colic and sigmoid arteries to form a continuous arterial channel, the marginal artery (juxtacolic artery). This artery parallels and extends the length of the colon close to its mesenteric border. The lymphatic drainage passes first to the epicolic and paracolic lymph nodes, next to the ileocolic and intermediate right colic lymph nodes, and from them to the superior mesenteric lymph nodes. The nerve supply to the ascending colon is derived from the superior mesenteric nerve plexus. The transverse colon is the third, longest, and most mobile part of the large intestine. It crosses the abdomen from the right colic flexure to the left colic flexure, where it turns inferiorly to become the descending colon. The left colic flexure (splenic flexure) is usually more superior, more acute, and less mobile than the right colic flexure. It lies anterior to the inferior part of the left kidney and attaches to the diaphragm through the phrenicocolic ligament. The transverse colon and its mesentery, the transverse mesocolon, loop down, often inferior to the level of the iliac crests. The mesentery is adherent to or fused with the posterior wall of the omental bursa.
Cheap nifedipine express
It ascends in the posterior mediastinum among the thoracic aorta on its left arteria pharyngea ascendens order generic nifedipine canada, the azygos vein on its right, the esophagus anteriorly, and the vertebral bodies posteriorly. At the level of the T4, T5, or T6 vertebra, the thoracic duct crosses to the left, posterior to the esophagus, and ascends into the superior mediastinum. The thoracic duct receives branches from the middle and superior intercostal spaces of both sides through several collecting trunks. Near its termination, the thoracic duct often receives the jugular, subclavian, and bronchomediastinal lymphatic trunks (although any or all these vessels may terminate independently). The thoracic duct usually empties into the venous system near the union of the left internal jugular and subclavian veins-the left venous angle or origin of the left brachiocephalic vein. There are several nodes posterior to the inferior part of the esophagus and more (up to eight) anterior and lateral to it. The posterior mediastinal lymph nodes receive lymph from the esophagus, the posterior aspect of the pericardium and diaphragm, and the middle posterior intercostal spaces. Lymph from the nodes drains to the right or left venous angles via the right lymphatic duct or the thoracic duct. The azygos system exhibits much variation in its origin, course, tributaries, and anastomoses. It ascends in the posterior mediastinum, passing close to the right sides of the bodies of the inferior 8 thoracic vertebrae. The azygos and hemiazygos veins are also continuous inferiorly (below diaphragm) with the ascending lumbar veins. The hemi-azygos vein arises on the left side by the junction of the left subcostal and ascending lumbar veins. It ascends on the left side of the vertebral column, posterior to the thoracic aorta as far as the T9 vertebra. The hemi-azygos vein receives the inferior three posterior intercostal veins, the inferior esophageal veins, and several small mediastinal veins. The accessory hemi-azygos vein begins at the medial end of the 4th or 5th intercostal space and descends on the left side of the vertebral column from T5 through T8. It crosses over the T7 or T8 vertebra, posterior to the thoracic aorta and thoracic duct, where it joins the azygos vein. The thoracic trunks lie against the heads of the ribs in the superior part of the thorax, the costovertebral joints in the midthoracic level, and the sides of the vertebral bodies in the inferior part of the thorax. The lower thoracic splanchnic nerves -also known as greater, lesser, and least splanchnic nerves-are part of the abdominopelvic splanchnic nerves because they supply viscera inferior to the diaphragm.
Buy generic nifedipine 20 mg line
The lymphatic drainage of the auricle is as follows: the lateral surface of the superior half of the auricle drains to the superficial parotid lymph nodes heart attack friend can steal toys 30 mg nifedipine buy fast delivery. The lateral third of this slightly Sshaped canal is cartilaginous and is lined with skin that is continuous with the auricular skin. The medial two thirds of the meatus is bony and lined with thin skin that is continuous with the external layer of the tympanic membrane. The ceruminous and sebaceous glands in the subcutaneous tissue of the cartilaginous part of the meatus produce cerumen (earwax). The tympanic membrane, approximately 1 cm in diameter, is a thin, oval semitransparent membrane at the medial end of the external acoustic meatus. This membrane forms a partition between the external acoustic meatus and the tympanic cavity of the middle ear. The tympanic membrane is covered with thin skin externally and mucous membrane of the middle ear internally. Viewed through an otoscope, the tympanic membrane has a concavity toward the external acoustic meatus with a shallow, cone-like central depression, the peak of which is the umbo. The central axis of the tympanic membrane passes perpendicularly through the umbo like the handle of an umbrella, running anteriorly and inferiorly as it runs laterally. Thus, the tympanic membrane is 2187 oriented like a mini radar or satellite dish positioned to receive signals coming from the ground in front and to the side of the head. The tympanic membrane has been rendered semitransparent and the lateral wall of the epitympanic recess has been removed to demonstrate the ossicles of the middle ear in situ. Superior to the lateral process of the malleus (one of the small ear bones, or auditory ossicles, of the middle ear), the membrane is thin and is called the pars flaccida (flaccid part). It lacks the radial and circular fibers present in the remainder of the membrane, called the pars tensa (tense part). The flaccid part forms the lateral wall of the superior recess of the tympanic cavity. The tympanic membrane moves in response to air vibrations that pass to it through the external acoustic meatus. Movements of the membrane are transmitted by the auditory ossicles through the middle ear to the internal ear. The skin of the superior and anterior walls of the external acoustic meatus and the supero-anterior two thirds of the external surface of the tympanic membrane are supplied mainly by the auriculotemporal nerve. Middle Ear the tympanic cavity or cavity of the middle ear is the narrow air-filled chamber in the petrous part of the temporal bone. The cavity has two parts: the tympanic cavity proper, the space directly internal to the tympanic membrane, and the epitympanic recess, the space superior to the membrane. The tympanic cavity is connected anteromedially with the nasopharynx by the pharyngotympanic tube and posterosuperiorly with the mastoid cells through the mastoid antrum. The tympanic cavity is lined with mucous membrane that is continuous with the lining of the pharyngotympanic tube, mastoid cells, and mastoid antrum. The axis of the tympanic membrane and the axis about which the cochlea winds runs inferiorly and anteriorly as it proceeds laterally.
Phet Sangkhat (Cissus Quadrangularis). Nifedipine.
- Obesity and weight loss, diabetes, metabolic syndrome, and high cholesterol, bone fractures, osteoporosis, scurvy, cancer, upset stomach, hemorrhoids, stomach ulcer, menstrual discomfort, asthma, malaria, pain, and body building.
- Dosing considerations for Cissus Quadrangularis.
- What is Cissus Quadrangularis?
- How does Cissus Quadrangularis work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97110
Nifedipine 30 mg buy on line
Fat-filled lateral and medial alar folds cover the inner surface of fat pads that occupy the space on each side of the patellar ligament internal to the fibrous layer blood pressure low heart rate high purchase 30 mg nifedipine mastercard. The synovial membrane of the joint capsule is continuous with the synovial lining of this bursa. This large bursa usually extends approximately 5 cm superior to the 1802 patella; however, it may extend halfway up the anterior aspect of the femur. Muscle slips deep to the vastus intermedius form the articularis genu, which attaches to the synovial membrane and retracts the bursa during extension of the knee. They are sometimes called external ligaments to differentiate them from internal ligaments, such as the cruciate ligaments. The patellar ligament, the distal part of the quadriceps femoris tendon, is a strong, thick fibrous band passing from the apex and adjoining margins of the patella to the tibial tuberosity. Laterally, it receives the medial and lateral patellar retinacula, aponeurotic expansions of the vastus medialis and lateralis and overlying deep fascia. The oblique placement of the femur and/or line of pull of the quadriceps femoris muscle relative to the axis of the patellar tendon and tibia, assessed clinically as the Q-angle, favors lateral displacement of the patella. The collateral ligaments of the knee are taut when the knee is fully extended, contributing to stability while standing. As flexion proceeds, they become increasingly slack, permitting and limiting (serving as check ligaments for) rotation at the knee. The cavity/synovial membrane extends superiorly deep to the 1804 quadriceps, forming the suprapatellar bursa. Tibial collateral ligament (isolated from the fibrous layer of the joint capsule, of which it is a part). It extends inferiorly from the lateral epicondyle of the femur to the lateral surface of the fibular head. The oblique popliteal ligament is a recurrent expansion of the tendon of the semimembranosus that reinforces the joint capsule posteriorly as it spans the intracondylar fossa. The ligament arises posterior to the medial tibial condyle and passes superolaterally toward the lateral femoral condyle, blending with the central part of the posterior aspect of the joint capsule. The arcuate popliteal ligament also strengthens the joint capsule posterolaterally. It arises from the posterior aspect of the fibular head, passes superomedially over the tendon of the popliteus, and spreads over the posterior surface of the knee joint. Its development appears to be inversely related to the presence and size of a fabella in the proximal attachment of the lateral head of gastrocnemius (see clinical box "Fabella in Gastrocnemius,". Both structures are thought to contribute to posterolateral stability of the knee.
Order nifedipine 30 mg line
The inferior laryngeal vein joins the inferior thyroid vein or the venous plexus of veins on the anterior aspect of the trachea blood pressure medication beginning with r discount nifedipine 30 mg with mastercard, which empties into the left brachiocephalic vein. The laryngeal lymphatic vessels superior to the vocal folds accompany the superior laryngeal artery through the thyrohyoid membrane and drain into the superior deep cervical lymph nodes. The lymphatic vessels inferior to the vocal folds drain into the pretracheal or paratracheal lymph nodes, which drain into the inferior deep cervical lymph nodes. The superior laryngeal nerve arises from the inferior vagal ganglion at the superior end of the carotid triangle. The nerves of the larynx are the internal and external branches of the superior laryngeal nerve and the inferior laryngeal nerve from the recurrent laryngeal nerve. The right recurrent laryngeal nerve passes inferior to the right subclavian artery. The internal laryngeal nerve, the larger of the terminal branches of the superior laryngeal nerve, pierces the thyrohyoid membrane with the superior laryngeal artery, supplying sensory fibers to the laryngeal mucous membrane of the laryngeal vestibule and middle laryngeal cavity, including the superior surface of the vocal folds. The external laryngeal nerve, the smaller terminal 2314 branch of the superior laryngeal nerve, descends posterior to the sternothyroid muscle in company with the superior thyroid artery. At first, the external laryngeal nerve lies on the inferior pharyngeal constrictor; it then pierces the muscle, contributing to its innervation (with the pharyngeal plexus), and continues to supply the cricothyroid muscle. The inferior laryngeal nerve, the continuation of the recurrent laryngeal nerve (a branch of the vagus nerve), enters the larynx by passing deep to the inferior border of the inferior pharyngeal constrictor and medial to the lamina of the thyroid cartilage. It divides into anterior and posterior branches, which accompany the inferior laryngeal artery into the larynx. The posterior branch supplies the posterior crico-arytenoid and transverse and oblique arytenoid muscles. Because it supplies all the intrinsic muscles except the cricothyroid, the inferior laryngeal nerve is the primary motor nerve of the larynx. However, it also provides sensory fibers to the mucosa of the infraglottic cavity. It transports air to and from the lungs, and its epithelium propels debris-laden mucus toward the pharynx for expulsion from the mouth. The trachea is a fibrocartilaginous tube, supported by incomplete cartilaginous tracheal cartilages (rings), that occupies a median position in the neck. The tracheal cartilages keep the trachea patent; they are deficient posteriorly where the trachea is adjacent to the esophagus. The posterior gaps in the tracheal rings are spanned by the involuntary trachealis muscle, smooth muscle connecting the ends of the rings. This sagittal 2316 section does not demonstrate the continuities of the upper respiratory tract because the soft palate is elevated, closing off the nasopharynx, and the plane of section passes through the vestibular and vocal folds to the side of the rima glottidis. The trachea extends from the inferior end of the larynx at the level of the C6 vertebra. Lateral to the trachea are the common carotid arteries and the lobes of the thyroid gland.
Discount nifedipine line
The deep bronchopulmonary lymphatic plexus is located in the submucosa of the bronchi and in the peribronchial connective tissue pulse pressure normal rate nifedipine 30 mg buy otc. It is largely concerned with draining the structures that form the root of the lung. Lymphatic vessels from this deep plexus drain initially into the intrinsic pulmonary lymph nodes, located along the lobar bronchi. Lymphatic vessels from these nodes continue to follow the bronchi and pulmonary vessels to the hilum of the lung, where they also drain into the bronchopulmonary lymph nodes. From them, lymph from 816 both the superficial and deep lymphatic plexuses drains to the superior and inferior tracheobronchial lymph nodes, superior and inferior to the bifurcation of the trachea and main bronchi, respectively. The right lung drains primarily through the consecutive sets of nodes on the right side, and the superior lobe of the left lung drains primarily through corresponding nodes of the left side. Many, but not all, of the lymphatics from the inferior lobe of the left lung, however, drain to the right superior tracheobronchial nodes; the lymph then continues to follow the right-side pathway. Lymph from the tracheobronchial lymph nodes passes to the right and left bronchomediastinal lymph trunks, the major lymph conduits draining the thoracic viscera. These trunks usually terminate on each side at the venous angles (junctions of the subclavian and internal jugular veins); however, the right bronchomediastinal trunk may first merge with other lymphatic trunks, converging here to form the short right lymphatic duct. Lymph from the parietal pleura drains into the lymph nodes of the thoracic wall (intercostal, parasternal, mediastinal, and phrenic). A few lymphatic vessels from the cervical parietal pleura drain into the axillary lymph nodes. These nerve networks contain parasympathetic, sympathetic, and visceral afferent fibers. After contributing to the posterior pulmonary plexus, the vagus nerves continue inferiorly and become part of the esophageal plexus, often losing their identity and then reforming as anterior and posterior vagal 818 trunks. Branches of the pulmonary plexuses accompany pulmonary arteries and especially bronchi to and within the lungs. They synapse with parasympathetic ganglion cells (cell bodies of postsynaptic neurons) in the pulmonary plexuses and along the branches of the bronchial tree. The parasympathetic fibers are motor to the smooth muscle of the bronchial tree (bronchoconstrictor), inhibitory to the pulmonary vessels (vasodilator), and secretory to the glands of the bronchial tree (secretomotor). Their cell bodies (sympathetic ganglion cells) are in the paravertebral sympathetic ganglia of the sympathetic trunks. The visceral afferent fibers of the pulmonary plexuses are either reflexive (conducting subconscious sensations associated with reflexes that control function) or nociceptive (conducting pain impulses generated in response to painful or injurious stimuli, such as chemical irritants, ischemia, or excessive stretch). Interalveolar connective tissue, in association with Hering-Breuer reflexes (a mechanism that tends to limit respiratory excursions).
30 mg nifedipine buy with mastercard
Seminal glands can be palpated during a rectal examination pre hypertension lifestyle changes order nifedipine 30 mg otc, especially if enlarged or full. They can also be massaged to 1408 release their secretions for microscopic examination to detect gonococci (organisms that cause gonorrhea), for example. An enlarged prostate projects into the urinary bladder and impedes urination by distorting the prostatic urethra. The middle lobule usually enlarges the most and obstructs the internal urethral orifice. The more the person strains, the more the valve-like prostatic mass obstructs the urethra. The prostate is examined for enlargement and tumors (focal masses or asymmetry) by digital rectal examination. A full bladder offers resistance, holding the gland in place and making it more readily palpable. In advanced stages, cancer cells metastasize both via lymphatic routes (initially to the internal iliac and sacral lymph nodes and later to distant nodes) and via venous routes (by way of the internal vertebral venous plexus to the vertebrae and brain). Because of the close relationship of the prostate to the prostatic urethra, obstructions may be relieved endoscopically. The instrument is inserted transurethrally through the external urethral orifice and spongy urethra into the prostatic urethra. In more serious cases, the entire prostate is removed along with the seminal glands, ejaculatory ducts, and terminal parts of the deferent ducts (radical prostatectomy). Seminal glands, ejaculatory ducts, and prostate: Obliquely placed seminal glands converge at the base of the bladder, where each of their ducts merges with the ipsilateral ductus deferens to form an ejaculatory duct. Thus, the major glandular secretions and sperms are delivered to the prostatic urethra. Female Internal Genital Organs the female internal genital organs include the ovaries, uterine tubes, uterus, and vagina. The mesovarium is a 1411 subdivision of a larger mesentery of the uterus, the broad ligament. Isolated dissection specimen consisting of the ovaries, uterine tubes, uterus, and related structures. This coronal section demonstrates the internal structure of the female genital organs. The epoophoron is a collection of rudimentary tubules in the mesosalpinx (mesentery of uterine tube). The epoophoron and vesicular appendage are 1412 vestiges of the embryonic mesonephros. In prepubertal females, the connective tissue capsule (tunica albuginea of the ovary) comprising the surface of the ovary is covered by a smooth layer of ovarian mesothelium or surface (germinal) epithelium, a single layer of cuboidal cells that gives the surface a dull, grayish appearance, contrasting with the shiny surface of the adjacent peritoneal mesovarium with which it is continuous. After puberty, the ovarian surface epithelium becomes progressively scarred and distorted because of the repeated rupture of ovarian follicles and discharge of oocytes during ovulation.
Ivan, 38 years: The main components of the nasal septum are the perpendicular plate of the ethmoid, the vomer, and the septal cartilage.
Navaras, 27 years: Skeleton of Thoracic Wall the thoracic skeleton forms the osteocartilaginous thoracic cage.
Ines, 26 years: Dural border hemorrhage is typically venous in origin and commonly results from tearing a superior cerebral vein as it enters the superior sagittal sinus.
Lukar, 34 years: Arrows indicate one of the biopsy needle tracks, at some distance from the neoplasm.
Bernado, 43 years: Deep lymphatic vessels from the leg accompany deep veins and also enter the popliteal lymph nodes.
Curtis, 51 years: The gluteal muscles (gluteus maximus, medius, and minimus and tensor fasciae latae) form the bulk of the region.
Nafalem, 64 years: The proximal end of the fibula consists of an enlarged head superior to a small neck.
Moff, 54 years: Rupture of the pancreas frequently tears its duct system, allowing pancreatic juice to enter the parenchyma of the gland and to invade adjacent tissues.
Rasarus, 56 years: Alimentary Layer of Cervical Viscera In the alimentary layer, cervical viscera take part in the digestive functions of the body.
Yussuf, 24 years: Thoracentesis Sometimes it is necessary to insert a hypodermic needle through an intercostal space into the pleural cavity (thoracentesis) to obtain a sample of fluid or to remove blood or pus.
Pakwan, 50 years: A gap between the superior and middle pharyngeal constrictors forms a passageway that allows the stylopharyngeus, glossopharyngeal nerve, and stylohyoid ligament to pass to the internal aspect of the pharyngeal wall.
Peer, 29 years: The 1st dorsal metatarsal artery divides into branches that supply both sides of the great toe and the medial side of the 2nd toe.
Ismael, 40 years: In the anatomical position, a line joining the tips of the greater trochanters normally passes through the pubic tubercles and the center of the femoral heads.
Armon, 21 years: Neck: narrow, tapering end, opposite the fundus and directed toward the porta hepatis; it typically makes an S-shaped bend and joins the cystic duct.
Killian, 52 years: Ventricles of brain: Each cerebral hemisphere includes a lateral ventricle in its core; otherwise, the ventricular system of the brain is an unpaired, median formation that communicates with the subarachnoid space surrounding the brain and spinal cord.
Asam, 31 years: The infection often develops in swimmers who do not dry their meatus (ear canals) after swimming and/or use ear drops.
Spike, 32 years: Flail chest is an extremely painful injury and impairs ventilation, thereby affecting oxygenation of the blood.
Stejnar, 46 years: The musculofibrous folds of the lips continue laterally as the cheek, which also contains the buccinator muscle and buccal fat-pad.
8 of 10 - Review by N. Khabir
Votes: 286 votes
Total customer reviews: 286