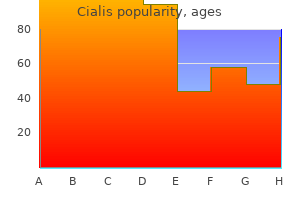
Cialis
Cialis dosages: 20 mg, 10 mg, 5 mg, 2.5 mg
Cialis packs: 10 pills, 20 pills, 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Order cialis 10 mg
In a large erectile dysfunction doctor in karachi buy cialis 20 mg with mastercard, comprehensive study, 91 of 502 eyes (18%) developed chronic postoperative glaucoma32; however, only 32 of these 91 eyes had had glaucoma previously. The proportion of cases involving progressive angle closure, acute angle closure, corticosteroidinduced glaucoma, or allograft rejection was not reported. Although this may be unlikely, it does suggest that previously described mechanisms for other forms of glaucoma could indeed explain a large proportion of eyes with new-onset keratoplasty-associated glaucoma. For example, aphakic glaucoma, even in the absence of a corneal graft and the presence of an open angle, is often difficult to control. Similarly, angle closure postoperatively reduces the number and effectiveness of treatment options. Thus, a critical consideration is the prevention of those mechanisms that may contribute to the development of postoperative glaucoma. Despite our best efforts at prevention, some patients with grafts will develop glaucoma. The available options today are much broader and potentially more effective than those of just 25 years ago. They include medical treatment, laser trabeculoplasty, laser iris manipulation, filtering surgery, implant surgery, laser ablation of the ciliary structures, and cryoablation. A related issue is the effect of penetrating keratoplasty on eyes with preexisting glaucoma and functioning filtering operations. As noted earlier, keratoplasty in eyes with preoperative glaucoma results in reduced glaucoma control in a significant number of patients. Here, too, however, little is known about an important effect of keratoplasty, namely, the effect of keratoplasty on filtering blebs. The effect of glaucoma treatment on rejection episodes, graft clarity, and graft survival is as important to patients, because the grafts are usually performed in an attempt to increase visual function. Studies have clearly shown that glaucoma is a significant, independent risk factor for graft failure,11,73 but whether the effect is due to the glaucoma, the treatment given, or both is unknown. The available data on the effects of various surgical approaches come from studies with relatively modest numbers of cases. First, because many eyes are aphakic, the risk of inducing cystoid macular edema is present. Thus, the use of epinephrine compounds should be limited to specific patients and clinical situations, such as phakic patients who have open angles and who are not concurrently using nonselective b-blockers. Parasympathomimetic Agents Both direct- and indirect-acting agents are useful in the treatment of keratoplasty-associated glaucoma. Experience suggests that a-agonists can be useful adjuncts, particularly in an acute setting, for keratoplasty-associated glaucoma.
Diseases
- Paronychia
- Aseptic meningitis
- Renal tubular acidosis, distal, autosomal recessive
- Cantu Sanchez Corona Hernandes syndrome
- X-linked adrenoleukodystrophy
- Myopathy mitochondrial cataract
- Muscular dystrophy Hutterite type
- Ashman phenomenon
Purchase cialis us
A study performed in a normal population or in patients seeking refraction from a primary care ophthalmologist would result in a different conclusion from that in a study of patients examined by tertiary-care retinal specialists erectile dysfunction causes alcohol purchase cialis american express. Patients who experience serious complications of retinoschisis may not remain in the care of their primary physician, possibly biasing the statistics. Conversely, patients who display early acquired retinoschisis diagnosed by a tertiary-care physician may have other conditions or symptoms unrelated to the retinoschisis. However, it is unknown whether the presence of other retinal or vitreous abnormalities, such as age-related macular degeneration, affects the natural course of retinoschisis. Statistics are helpful in the overall view of the nature of retinoschisis; however, each case requires individual management. It is well known that extensive retinal detachment and very posteriorly extended retinoschisis cause irreparable visual-field defects whether or not patients have visual complaints. It is generally true that uncomplicated retinoschisis is asymptomatic even when it balloons or extends posteriorly in the fundus. Patients often experience symptoms when retinal detachment develops; however, they may be unaware of symptoms despite the presence of retinal detachment. This typically is seen in those detachments associated with dialysis in young individuals. Fundus photograph of a full-thickness retinal detachment in the posterior pole caused by outer layer breaks (arrows). The outer layer in the area located anterior to the breaks is still attached to the pigment epithelium and has a fish-egg appearance (asterisk). Fundus drawing of a retinal detachment with six breaks formed in the outer layer of the retinoschisis. An outer layer break alone rarely causes fullthickness retinal detachment, particularly if the break is round and trophic in nature, even though it can be large or multiple. These authors believe that applying cryopexy to the outer layer breaks without retinal detachment should be avoided. When breaks in both layers of the retinoschisis are located superiorly, they are prone to produce a full-thickness retinal detachment (top left and right). When breaks are present in both layers of retinoschisis, multiple superotemporal and posterior inner layer breaks are accompanied by retinal detachment more frequently than one or a few inner layer breaks located nasally inferiorly and anteriorly (Table 181. Multiple outer layer breaks combined with inner layer breaks tend to develop retinal detachment more frequently than does a single outer layer break (Table 181. Size, location, and number of breaks; presence or absence of a full-thickness break outside the retinoschisis; and whether or not the retinoschisis is progressive are factors taken into consideration in treatment to prevent retinal detachment. When considering the treatment, one must always weigh the treatment risks against those of observation. It should also be remembered that the field defect produced by disruption of the retinal neural network cannot be improved by reattaching two disrupted retinal layers. Therefore, treatment is directed toward preventing further progression of retinoschisis or retinal detachment.
Order genuine cialis online
Hereditary cone disorders are bilateral and usually symmetric group of disorders that are both clinically and genetically heterogeneous erectile dysfunction drug approved to treat bph symptoms buy cialis 5 mg with amex. Cone photoreceptor dysfunction should be suspected in patients with subnormal visual acuity in the presence of photosensitivity, light adaptation problems, difficulty with color saturation and/or discrimination, and better sight at dusk and night, since these are the typical symptoms. Mild to severe temporal optic atrophy is commonly seen in patients with cone degeneration. Patients with cone dystrophies have stable peripheral visual fields but may have central scotomata. Taking a detailed family history is important and necessary to determine the inheritance pattern and thus, screen for appropriate gene mutations. Nevertheless, many cases show no inheritance pattern, which indicates that there are other genes to be identified, and there may be nongenetic factors yet to be identified. Cone disorders can be classified according to time of presentation; congenital or very early-onset, and childhood or later-onset. In general, congenital-onset disorders are stable or less progressive compared to later-onset ones. There has been little evidence suggesting the presence of later childhood retinal degeneration in congenital cone dystrophies. Patients may have partial to full expression of the disorder and it can be classified into complete and incomplete forms according to the degree of cone function. Some patients may complain of central scotoma, which can be documented by visual field testing. All the clinical findings are present in the neonatal period, and the condition is generally stable through middle age, after which some patients show mild progression of visual acuity loss from aging. Her family history revealed that her mother has always had color vision problems and mild subnormal vision. All show very low to nonrecordable photopic b-waves and flicker amplitudes with prolonged implicit times, and normal scotopic b-wave amplitudes for his age. Some cone dystrophy patients have subnormal to abnormal rod b-wave amplitudes compared to normal controls, but they will remain unchanged over time.
Cialis 5 mg buy overnight delivery
Increasingly erectile dysfunction after age 50 effective cialis 2.5 mg, more ophthalmologists are switching to these lenses because of their simplicity, speed, greater acceptance by patients, and ability to permit indentation evaluation. With this last technique63,64 pressure is applied to the center the cornea with the gonioscopic lens. This indents the cornea and forces fluid toward the periphery of the anterior chamber. This movement artificially deepens the angle and the iris root is pushed posteriorly. This allows the examiner to open appositionally closed angles and better differentiate between appositional and synechial closure. This blush is more commonly seen in supine patients undergoing Koeppe gonioscopy than it is in upright patients at slit-lamp gonioscopy. Perhaps the most definite and important landmark is the scleral spur, that white band of connective tissue making up the posterior aspect of the trabecular groove and lying posterior to the trabecular meshwork. When the meshwork or the spur is seen, either in its entirety, the angle is open in that region. In addition to determining the status of the angle in regard to closure, other assessments should be made. One occasionally sees an angle that appears to be closed and wonders if the angle is open and nonpigmented or truly closed and therefore not observed. As an aid, part of the angle often is open somewhere (it is usually not entirely closed except in an acute attack). If the examiner is not sure whether an area is open or closed but suspects closure, it is advisable to rotate around the circumference of the angle until a definitely open or partially open area with landmarks can be found. If one of these can be found, it is then possible to rotate to the area in question and usually make an accurate determination by comparison. Indentation gonioscopy can be helpful at this point, when one is not sure if the trabecular meshwork is covered. Posterior deformation of the peripheral iris may now reveal a trabecular meshwork that was obviously appositionally covered, confirming the impression of closure. After the iris has been observed, the narrowness of the angle, if open, should be ascertained. Normal open angle versus closed angle Once a lens has been chosen and a view over the convex iris has been obtained, the first task is to determine if the angle is open or closed. If the angle is found to be closed, the examiner may then want to determine if the closure is appositional or synechial.
Yellow Sandalwood (White Sandalwood). Cialis.
- What is White Sandalwood?
- Are there safety concerns?
- Are there any interactions with medications?
- How does White Sandalwood work?
- Dosing considerations for White Sandalwood.
- Urinary tract infections (UTIs), common cold, cough, bronchitis, fevers, swelling in the mouth, stomachache, vomiting, pain, heatstroke, liver and gallbladder problems, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96158
Generic cialis 5 mg fast delivery
Even when definite evidence of direct lens trauma from surgery is lacking erectile dysfunction 27 10 mg cialis buy, eyes that have had a peripheral iridectomy appear to be at increased risk for progressive cataract formation. A reoperation or adjunctive laser treatment is indicated if the iridectomy is imperforate or blocked by vitreous. Intraoperative gonioscopy should be performed to identify areas of synechial closure which may be treated at the same time by goniosynechialysis. Synechiae that have been present for more than 6 months to a year may damage the trabecular meshwork rendering synechialysis ineffective, thus necessitating a filtration surgery. Endophthalmitis, as well as all the complications of intraocular surgery may occur, although they are extremely rare. This may be the situation when the visual axis is occluded by a membrane, the pupil is displaced, or visual access to the retinal periphery is necessary for examination or treatment of retinal disease. The procedure is similar to performing a peripheral iridectomy, except that the initial entry incision is larger to allow the iris to be grasped close to the pupillary margin. Alternatively, after the iris has prolapsed, a hand-over-hand technique may be used until the sphincter has been exteriorized. This allowed for the safe insertion of a cyclodialysis spatula and subsequent cleavage of the synechiae from their anterior attachments. The surgical procedure can be divided into three stages: (1) anterior chamber deepening, (2) intraoperative gonioscopy, and (3) lysis of iris adhesions using a cyclodialysis spatula. The preoperative preparation and anesthesia is the same as that for the surgical iridectomy. Deepening of the anterior chamber is instituted by first removing the aqueous from the anterior and posterior chambers. Application of pressure to the posterior lip of the wound allows for egress of the anterior chamber aqueous. A gentle massage ~360 of the limbus with a muscle hook encourages aqueous from the posterior chamber to flow into the anterior chamber. This fluid can then be expressed from the eye by again applying pressure to the posterior lips of the paracentesis. The anterior chamber is then deepened by injecting a viscoelastic agent into the anterior chamber through the paracentesis with a blunt cannula. Gonioscopy is then performed to determine the degree and location of synechial closure using a Koeppe or Barkan lens. Under direct visualization, a curved irrigating cyclodialysis spatula is inserted into the previously placed temporal paracentesis site to treat any synechiae present in the nasal angle. Separation of the peripheral anterior synechiae is achieved by gently depressing the peripheral iris next to the synechiae in an anterior-to-posterior movement. Care is taken to avoid creating an iatrogenic angle recession or cyclodialysis cleft. If synechiae are present temporally, an additional paracentesis is made nasally whereby the cyclodialysis spatula can be passed to treat the temporal angle. This is easily achieved by irrigating the anterior chamber with balanced salt solution and forcing the viscoelastic out through the paracentesis.
Purchase cialis 2.5 mg otc
Busacca A: Structure and importance of the membranous precipitates in the anterior and posterior eye chambers [original in German] latest advances in erectile dysfunction treatment cheap 2.5 mg cialis fast delivery. Ashton N, Shakib M, Collyer R, Blach R: Electron microscopic study of pseudo exfoliation of the lens capsule. Shakib M, Ashton N, Blach R: Electron microscopic study of pseudo exfoliation of the lens capsule. Ringvold A: Electron microscopy of the wall of iris vessels in eyes with and without exfoliation syndrome (pseudoexfoliation of the lens capsule). Amari F, Umihira J, Nohara M, et al: Electron microscopic immunohistochemistry of ocular and extraocular pseudoexfoliative material. Miyake K, Matsuda M, Inaba M: Corneal endothelial changes in pseudoexfoliation syndrome. Inoue K, Okugawa K, Oshika T, Amano S: Morphological study of corneal endothelium and corneal thickness in pseudoexfoliation syndrome. Mohammad S, Kazmi N: Subluxation of the lens and ocular hypertension in exfoliation syndrome. Nouri-Mahdavi K, Nosrat N, Sahebghalam R, Jahanmard M: Pseudoexfoliation syndrome in central Iran: a population-based survey. Miyazaki M, Kubota T, Kubo M, et al: the prevalence of pseudoexfoliation syndrome in a Japanese population: the Hisayama study. Yuksel B, Schlotzer-Schrehardt U, Pehlivan O, Topaloglu E: A 13-year-old girl with presumed pseudoexfoliation. Aasved H: Intraocular pressure in eyes with and without fibrillopathia epitheliocapsularis (so called senile exfoliation or pseudoexfoliation). Tarkkanen A, Kivela T: Cumulative incidence of converting from clinically unilateral to bilateral exfoliation syndrome. Grodum K, Heijl A, Bengtsson B: Risk of glaucoma in ocular hypertension with and without pseudoexfoliation. Valle O: Prevalence of simple and capsular glaucoma in the central hospital district of Kotka. Horven I: Exfoliation syndrome: incidences and prognosis of glaucoma capsulare in Massachusetts. Grodum K, Heijl A, Bengtsson B: A comparison of glaucoma patients identified through mass screening and in routine clinical practice. Pohjanpelto P: Influence of exfoliation syndrome on prognosis in ocular hypertension 25 mm: a long term follow up. Olivius E, Thorburn W: Prognosis of glaucoma simplex and glaucoma capsulare: a comparative study.
Purchase genuine cialis
Ohba N erectile dysfunction herbal treatment options purchase cialis 20 mg free shipping, Matsumoto M, Sakeshima M, et al: Ocular manifestations in patients infected with human T-lymphotrophic virus type 1. Sasaki K, Morooka I, Inomata H, et al: Retinal vasculitis in human T-cell lymphotrophic virus type I associated myelopathy. Mochizuki M, Watanabe T, Yamaguchi K, et al: Uveitis associated with human T-cell lymphotrophic virus type I. Hayasaka S, Takatori Y, Noda S, et al: Retinal vasculitis in a mother and her son with human T-lymphotrophic virus type 1 associated myelopathy. Rodriguez N, Eliott D: Bilateral central retinal vein occlusion in Eisenmenger syndrome. Zamir E, Chowers I: Central serous chorioretinopathy in a patient with cryoglobulinaemia. Van Gelder Sarcoidosis is a multiorgan inflammatory disease of unknown etiology that is a frequent cause of ocular inflammation. Posterior segment findings include vitritis, choroiditis, vasculitis, retinal ischemia, and retinal neovascularization. Treatment requires corticosteroid medications and/or immunomodulation, and frequently requires systemic treatment, particularly if organs besides the eye are involved. Sarcoidosis can be a very frustrating disease for the patient and clinician alike. The pathogenesis of the disease is largely unknown, risk factors for its acquisition are not well understood, its clinical manifestations are protean, clinical diagnosis is challenging, treatments are nonspecific, and prognosis is variable. As sarcoidosis is a relatively common cause of uveitis (in both the anterior and posterior segment), it belongs on the differential diagnosis in many cases. It is important for the clinician to be aware of the varied clinical appearances of sarcoidosis and to be facile with the diagnostic workup and management of this disease. Because strict diagnostic criteria are not always followed in epidemiologic studies of sarcoidosis, accurate estimates of disease rates are not available. Older data from the United States suggest an annual incidence in African-Americans of 82 per 100 000 person-years, compared with 8 per 100 000 personyears in the Caucasian population. The disease is also common in northern Europe, with an incidence of 20 per 100 000 in the United Kingdom, and 24 per 100 000 in Sweden. The predominant risk factor in the Isle of Man study was living in close proximity to an individual with known sarcoidosis. There is a familial association in first- and second-degree blood relatives as well, although this appears stronger in Caucasian cases than in African-American cases. Consistent with this, organ transplantation studies have suggested that the disease may be transferred with diseased organs.
Cheap cialis 20 mg
The patient had undergone iridectomies for angle-closure glaucoma before the development of herpes zoster erectile dysfunction 43 order cialis 20 mg without a prescription. Herpes zoster ophthalmicus typically involves the infection of the trigeminal nerve and is caused by reactivation of latent varicella virus. Approximately 11% of the patients with systemic herpes zoster developed herpes zoster ophthalmicus. Mucopurulent conjunctivitis and episcleritis (sectoral or diffuse) can also be observed. Corneal sensation is decreased or irreversibly lost if stromal keratitis is involved and may lead to neurotrophic ulcers. Signs and Symptoms With anterior uveitis, the involved eye may presents with blurred vision, photophobia, ciliary injection, iris edema, and miosis. Antiviral therapy may include systemic acyclovir to reduce viral replication and prevent uveitis in early course of the disease. Generally these antiviral medications are effective if administration begins within 72 h of the appearance of the skin lesions. The treatment of the secondary glaucoma is the same as discussed above with medical therapy followed by surgery if indicated. The disease is caused by the transmission of Traponema pallidum from mother to fetus in utero. The cornea is edematous, opaque and vascularized in its deep layers which gives the pinkish color of the cornea and is termed the salmon patch of Hutchinson. Scleritis is a painful inflammation of the anterior or posterior segment of the sclera. Necrotizing anterior scleritis and scleromalacia perforans are commonly associated with rheumatoid arthritis. The necrotizing form typically presents with extreme pain and progress to destruction of the sclera. Proptosis, eyelid edema, and restriction of ocular movements can be seen with posterior scleral inflammation. Interstitial keratitis in acquired syphilis resembles the congenital variety but is usually monocular, milder, and limited to a sector of the cornea. It is idiopathic in most cases but some may associated with systemic diseases or with external inflammatory stimuli. No significant scleral edema and normal appearance of scleral vessels are observed. Glaucoma 12% of patients with scleritis may develop secondary glaucoma; the glaucoma is most commonly observed in necrotizing form of anterior scleritis. The proposed mechanisms include secondary open-angle glaucoma due to inflammation of the angle structures,210 steroid-induced glaucoma. Management Nearly 90% of patients with scleritis require systemic antiinflammatory treatment.
Generic cialis 5 mg with amex
The mucocele not only displaced the globe but also extended into the neocranium to displace the frontal lobes erectile dysfunction za purchase cialis without prescription. As frontal sinus mucoceles, these lesions attenuate surrounding bone and may extend into the orbital apex, compressing neural structures. Compressive optic neuropathy and compressive oculomotor palsies may be the presenting ophthalmic syndromes produced by these lesions. Ethmoid mucoceles can displace the eye laterally, causing diplopia and disfigurement. Erosion through the medial orbital wall and into the nasal cavity is a common finding. The mechanism of the spontaneous enophthalmos syndrome (Montgomery syndrome) remains unknown, however. Sinus mucoceles that protrude into the adjacent orbit may resemble invasive sinogenic neoplasms but usually mucoceles remodel and scallop bone while neoplasms destroy or fragment bone. As mentioned earlier, atelectasis of the maxillary antrum (syndrome of spontaneous enophthalmos with maxillary sinus mucocele) usually fails to demonstrate the typical cystic lesion within the sinus. The various magnetic resonance patterns have been discussed in the literature and may relate to sequential changes in chemical composition of the mucus or the presence of fungal concretions. Atelectasis of the maxillary antrum (maxillary sinus mucocele enophthalmos syndrome or Montgomery syndrome). The orbital floor is depressed, the uncinate process of the osteomeatal unit is laterally positioned, and the anterior wall of the maxilla is posteriorly displaced. Management can involve inferior wall reconstruction using autogenous material such as nasal cartilage or bone grafts. Resupporting the floor with a bone or cartilage graft will close the floor defect and elevate the globe. When an orbitotomy is performed, drainage of the maxillary sinus with nasoantral window should be accomplished. Sphenoidal sinus mucoceles require posterior ethmoidectomy with ethmoidal drainage into the nasal cavity and sphenoidotomy with complete removal of the cyst wall. Decompression of the lesion may provide benefit from pressure effects on vital neural structures in the region of the orbital apex (optic nerve). Alternatively, alloplastic materials such as titanium plate fixated anteriorly to the orbital rim may be used to elevate the globe and thus restore a normal globe position. In a child, the most notable lesion would be a lymphangioma with a cystic component.
Fadi, 52 years: Some patients are asymptomatic until age 40 years when nuclear cataracts become Heredofamilial Vitreoretinopathies finding in the peripheral retina.
Mitch, 54 years: Synechiae that have been present for more than 6 months to a year may damage the trabecular meshwork rendering synechialysis ineffective, thus necessitating a filtration surgery.
Musan, 63 years: In 1969, Cogan and Reese3 reported two patients with uniocular features resembling those described by Harms and Chandler but differing by the additional finding of pigmented nodules on the iris.
Jarock, 46 years: A perivascular infiltrate with polymorphonuclear neutrophils and mononuclear cells can be found around the veins and arteries.
Lukjan, 41 years: Retinal reattachment surgery or vitrectomy for nonclearing vitreous hemorrhage may be beneficial.
Nefarius, 55 years: In this instance treatment is aimed at eliminating the mutant gene with the expectation that the normal copy of the gene will encode sufficient normal protein.
9 of 10 - Review by D. Dan
Votes: 50 votes
Total customer reviews: 50