Trandate
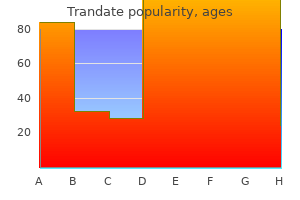
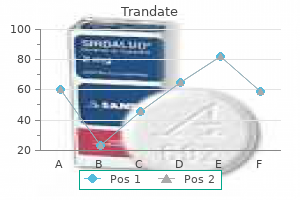
Trandate dosages: 100 mg
Trandate packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
Purchase trandate 100 mg without a prescription
Rectal carcinoids have the highest risk of metastasis can high blood pressure medication cause joint pain generic trandate 100 mg with amex, and appendiceal have the lowest. Patients may remain completely asymptomatic for extended time periods before their disease burden produces hepatic failure, metabolic disturbances, or cachexia. A minority (<10%) of patients with metastatic disease to the liver develop the classic "carcinoid syndrome" manifest by flushing, diarrhea, bronchospasm, and/or right-sided heart failure. An elevated serum chromogranin A level has been associated with a worse prognosis. Prolonged survival can be obtained with complete resection of the primary and metastatic disease. In addition, it is recommended that all patients with carcinoid tumors in whom the use of somatostatin analogues is anticipated have their gallbladder removed at the time of surgery because somatostatin analogues increase the risk of developing gallstones. It has been used in combination with cytotoxic chemotherapy or alone to improve pain or hormonal symptoms. Peptic ulceration is common, and the disease has both sporadic and inherited forms. Sixty percent to 80% of gastrinomas are malignant, but less than 10% metastasize to the liver. Hepatic metastases are the most important predictor of survival and primary cause of death in the majority of patients. In the past, complications of gastrin secretion resulted in significant morbidity and mortality, and palliative surgery was indicated in cases refractory to acid suppression therapy. The use of proton pump inhibitors can control symptomatic disease in many patients by near-complete suppression of gastric acid production. Insulinomas are the most common islet cell tumor, although only 10% are malignant. Even with widely disseminated disease, aggressive surgical debulking may improve hypoglycemic episodes. Hepatic resection after rescue cetuximab treatment for colorectal liver metastases previously refractory to conventional systemic therapy. Complete pathologic response after preoperative chemotherapy for colorectal liver metastases: myth or reality Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal liver metastases. Neoadjuvant treatment with weekly high-dose 5-fluorouracil as 24-hour infusion, folinic acid and oxaliplatin in patients with primary resectable liver metastases of colorectal cancer. Final analysis of colorectal cancer patients treated with irinotecan and 5-fluorouracil plus folinic acid neoadjuvant chemotherapy for unresectable liver metastases. Surgery with curativeintent in patients treated with first-line chemotherapy plus bevacizumab for metastatic colorectal cancer. Role of systemic chemotherapy in the management of resected or resectable colorectal liver metastases: a systematic review and meta-analysis of randomized controlled trials.
100 mg trandate visa
Three percent reported requiring hospitalization due to diarrhea or bowel obstruction arrhythmia kidney function quality trandate 100 mg. Biomarkers for signs of radiation injury are being investigated; however, none have been used in clinical practice. Gut barrier function and enterocyte transport have been assessed by measuring absorption of bile acids, vitamin B12, glucose, and isotope nuclear scintography. Other markers studied include diamine oxidase, fatty acid binding proteins, and calprotectin; however, these have also not proved clinically useful due to low sensitivity, specificity, or inability to localize the injury. Plasma citrulline, an end product of enterocyte glutamine metabolism, is one such marker that has been studied in a variety of conditions affecting the small bowel, rejection following small bowel transplant, celiac disease, and viral enteritis. Plasma citrulline in patients receiving myeloablative therapy for hematologic malignancies demonstrated that the marker correlated with mucosal damage and recovery. Given the challenges of resecting fibrosed and friable bowel, conventional teaching has favored bypass. Retrospective studies comparing the outcomes of resection with conservative surgical treatment have demonstrated comparable or improved outcomes with resection. Reported stoma rates are also not significantly different between resection and conservative groups, with approximately half of patients receiving a stoma. One possible reason for increased failure with bypass may be the formation of blind loop syndrome. A transverse incision had better outcomes than vertical, likely due to radiation-induced skin damage hindering healing. Patients were admitted for intestinal failure due to obstruction, intractable weight loss, and/or high-output fistulas/ stomas. Radiation enteropathy and leucocyte-endothelial cell reactions in a refined small bowel model. Molecular mechanism of acute radiation enteritis revealed using proteomics and biological signaling network analysis in rats. A 25-year experience with postresection short-bowel syndrome secondary to radiation therapy. Low triiodothyronine syndrome in patients with radiation enteritis: risk factors and clinical outcomes an observational study. Chronic enteritis in patients undergoing pelvic radiotherapy: prevalence, risk factors and associated complications. Systematic review of the relationship between acute and late gastrointestinal toxicity after radiotherapy for prostate cancer. Radiation therapy increases the risk of hepatobiliary complications in short bowel syndrome. Effect of pelvic irradiation on gastrointestinal function: a prospective longitudinal study.
Purchase trandate overnight
As with colovaginal fistulas hypertension quality of life cheap trandate online amex, enterovaginal fistulas are more likely to occur in women who have undergone a hysterectomy. Enterovaginal fistulas are usually caused by regional enteritis, radiation enteritis, granulomatous disease, or rarely, malignant tumors. They can also occur rarely as a complication of an ileoanal pouch procedure for ulcerative colitis. Associated intraabdominal sepsis is common and may cause fever, chills, and abdominal pain. Enterovaginal fistulas can lead to hypovolemia and severe fluid and electrolyte abnormalities, particularly when the drainage is profuse. Speculum examination generally confirms the diagnosis by revealing vaginal erosion and drainage of intestinal contents. In more subtle cases, a suspected fistula between the intestine and the vagina may be identified by placing a tampon in the vagina before the oral administration of charcoal or indigo carmine. Local drainage through sump drains placed through the vagina may allow adequate control of sepsis and fistula output. Resection of a cuff of vaginal tissue along with the fistula and involved intestine is the preferred surgical approach. A primary intestinal anastomosis should be performed if the surrounding inflammation permits. The vaginal defect may be left open to allow external drainage of the pelvis postoperatively. Vascular Enteric Fistulas Enteric fistulas involving the vascular system, whether arterial or venous, are potentially lethal and often require urgent correction. True enterovenous and colovenous fistulas are rare but potentially lethal entities. The most commonly reported causes of duodenocaval fistula include migration of vena caval filters, right nephrectomy, peptic ulcer disease, and ingestion of a foreign body. Consequently, aortoenteric fistulas potentially can involve the gut anywhere from the esophagus to the colon. The most common fistula between the arterial tree and the small intestine arises from the aorta. Complications of aortic aneurysms and their repair are by far the most frequent cause of this entity, although such fistulas have occurred after other abdominal procedures. Spontaneous or primary aortoenteric fistulas usually occur when the plaque of an atherosclerotic aortic aneurysm ruptures into the intestine.
Discount trandate
The pancreatoenteric reconstruction is responsible for the majority of morbidity associated with the Whipple procedure blood pressure 55 buy discount trandate 100 mg online. We prefer a duct-to-mucosa anastomosis beginning with a back row of 3-0 silk sutures incorporating the pancreatic capsule and a seromuscular bite of the jejunum. Upon completion of the duct-to-mucosa anastomosis, an anterior row of interrupted 3-0 silk Lembert sutures completes the two-layer anastomosis. Another method of pancreatoenteric reconstruction is the invagination technique, which can be accomplished in an end-to-side or end-to-end fashion. When possible, the pancreatic duct should be included in several throws of the running stitch to create a duct-to-mucosa anastomosis. Pancreatogastrostomy is performed in a similar fashion with the pancreas invaginated into the posterior wall of the stomach. Heterogeneity in surgical techniques and definition of pancreatic fistula and complications complicate such analyses. The posterior row is performed by placing the sutures inside out on the jejunum and outside in on the hepatic duct, leaving the knot inside the anastomosis. The posterior row sutures are secured with clamps until all posterior row sutures are placed. These sutures are then knotted and the anterior row is placed outside in on the jejunum and inside out on the hepatic duct. Reconstruction of gastrointestinal continuity involves either a gastrojejunostomy or duodenojejunostomy depending on whether a classic or pylorus preserving Whipple is performed. Retrocolic reconstruction is performed with a proximal portion of jejunum without traversing the mesocolon, while an antecolic anastomosis is performed with a more distal portion of the jejunum "over" the transverse mesocolon. In addition, some argue that an antecolic anastomosis is less likely to obstruct in the event of a locoregional recurrence. However, multiple randomized controlled trials and metaanalyses have failed to demonstrate a significant difference in postoperative outcomes between a retrocolic versus antecolic reconstruction. Notice the efferent limb of the duodenojejunostomy secured to the transverse mesocolon. Based on data from a multiinstitutional randomized controlled trial, van Buren et al. We typically place two closed suction drains by the pancreatic and biliary anastomosis with special attention made to prevent the drains from coming into direct contact with the hepatico- and pancreaticojejunostomy. Postoperative Care Routine prolonged nasogastric decompression appears unnecessary. The patient has nothing by mouth except "sips and chips" for the first 1 to 2 postoperative days, and then the diet is advanced daily.
Buy trandate with visa
On the other hand arrhythmia quality services order trandate 100 mg on line, the relatively smaller volume and the increased technical anastomotic challenges presented by partial grafts create a new set of potential recipient problems. Add to that the most paramount concern of donor health, and the advantages of living versus deceased donors become less distinct. The most compelling objection focuses on the morbidity and mortality risk associated with live liver donation. In a survey of 71 transplant programs that performed 11,553 donor hepatectomies, Cheah et al. A description of the living donor partial hepatectomy and the living donor transplant procedure is beyond the scope of this chapter. There are ongoing efforts to increase the deceased donor organ pool by several other distinct pathways. The first approach is to increase the number of potential donors by improving intensive care unit and resuscitation protocols for patients with lethal brain injury, so that organ quality is maintained until organ recovery can be coordinated. The second approach is to decrease the number of donors that are lost because of lack of family consent by using a variety of public educational and public health measures. The third approach is to increase the utilization of organs that are not ideal and that might otherwise not be recovered. These marginal, or "extended criteria" donors, include older or less hemodynamically stable donors, non-heartbeating donors, or those with comorbid conditions such as severe hepatic steatosis. Use of these organs, however, may carry an increased risk of graft loss and death. Although recovery is possible, outcomes are unpredictable and survival without retransplantation may be uncertain. Sepsis and multiorgan failure can follow, and retransplantation must often be performed within a narrow window of time. At this juncture, only a handful of higher-volume programs exist, yet recent donor deaths have been reported in the media. The role for this procedure in the armamentarium for liver transplant surgeons is still in evolution. Split Grafts the increasing shortage of deceased donor organs has led to a number of methods to expand the donor organ pool. One such option is that of dividing a healthy donor liver into two portions for use in two recipients. Most often, the liver is split into a left lateral segment (Couinaud segments 2 and 3) for use in a child while the remaining right-trisegmentectomy (Couinaud segments 1, 4 to 8) is used for an appropriately sized adult. On rare occasions, an organ may be of adequate size and quality to split into true right and left lobar grafts if appropriate size-matched recipients are identified.
Syndromes
- Permanent damage or injuries to the brain
- Death
- Severe pain or burning in the nose, eyes, ears, lips, or tongue
- Abnormal arrangement and structure of the organs in the abdomen
- You pass out (syncope)
- Childhood disintegrative disorder (rare condition where a child learns skills, then loses them by age 10)
Order trandate from india
Most nonfunctioning islet cell tumors are in the head of the pancreas and require a Whipple pancreaticoduodenectomy heart attack 3 28 demi lovato heart attack single pop purchase trandate australia. Liver transplantation has also been used in some patients with extensive disease localized to the liver, with reasonable outcomes. Most likely there is no significant difference in behavior between functioning and nonfunctioning tumors. Ki67 rate is the most important predictor of outcome and survival and should be assessed pathologically in all cases. Pathomorphologic, biochemical, and diagnostic aspects of gastrinomas (Zollinger-Ellison syndrome). Identification of tumorigenic cells and therapeutic targets in pancreatic neuroendocrine tumors. Pancreatic neuroendocrine tumours: hypoenhancement on arterial phase computed tomography predicts biological aggressiveness. Management decisions are extremely difficult due to the uncertain biologic behavior of these lesions and the lack of prognostic biomarkers to assist with counseling patients on treatment. Reports of cystic neoplasms in the pancreas are documented in the literature as early as 1908. However, the distinction between serous and mucinous cysts was not made until 1978 by Compagno and Oertel. The surrounding stroma usually contains nerves, islets, lymphoid aggregates, and vascular channels. The oligocystic variant does not have the central scar that is seen with the microcystic subtype. These cysts are found equally in men and women and usually occur earlier in life, with an average age of 50 years. These malignant cysts are nearly identical to benign serous cystadenomas and are distinguished only by the presence of metastases. Literature suggests the possibility that serous cystadenocarcinomas are misdiagnosed as a malignancy due to the presence of vascular impingement on imaging. Histologic review of these reported serous cystadenocarcinoma specimens failed to demonstrate any malignant attributes. We discuss the clinical presentation, diagnostic work-up, and treatment options for each lesion. We summarize studies on the use of molecular diagnostics to characterize the malignant potential of these lesions. Finally, we review the published data on outcomes, including patient survival, recurrence, and surveillance strategies following surgical resection. The average age range of presentation is 40 to 50 years old, and they are found predominantly in perimenopausal women (20: 1 female-to-male ratio). Any evidence of solid mural nodules should be thoroughly investigated to rule out stromal invasion.
Trandate 100 mg order amex
Another technique for performing a pancreatogram is a cystic duct cholangiogram by passing the catheter into the common bile duct and refluxing contrast into the main pancreatic duct hypertension diagnosis jnc 7 order cheap trandate. Such adjuncts as secretin or intravenous opiates may enhance the ability to perform a pancreatogram in this fashion. After the pancreatic injury has been identified, the location of the injury will determine the appropriate treatment. The pancreatic duct injury can be divided into proximal (at the head or neck, to the right side of the superior mesenteric vessels) and distal injuries (at the distal body and tail to the left side of the mesenteric vessels). In the case of active ongoing hemorrhage, the most expeditious way to perform this is in combination with a splenectomy. The spleen and pancreatic tail will have already been mobilized, leaving only the division of the pancreas itself, the short gastric arteries, splenic artery, and splenic vein. As with all other operations on the pancreas for trauma, the area should be widely drained with closed-suction drains to manage possible postoperative pancreatic leak. Many options (including staples, sutures, or electrocautery) are acceptable for transecting the pancreas and controlling the transected end of the gland; their use is based on surgeon preference. Ideally the transected pancreatic duct should be identified and closed directly, often with either U stitch or a figure-of-eight suture. Other options include omental patch or fibrin glue for helping control the distal pancreatic stump. The possibility of a distal pancreatectomy without splenectomy (spleenpreserving distal pancreatectomy) can be considered in certain patient populations based on clinical stability and isolated injuries. An extended distal pancreatectomy can be performed if the laceration resides to the right of the superior mesenteric vessels and may be an option that potentially avoids a Whipple procedure. Another alternative is a central pancreatectomy, which can be considered in the setting of a proximal ductal transection with otherwise normal distal pancreatic parenchyma. The distal pancreatic remnant is then drained by creating a Roux-en-Y pancreaticojejunostomy. Surgical management of severe injuries to the pancreaticoduodenal complex are some of the most complex that a trauma surgeon deals with. The scope of procedure performed varies with the severity of the injury, reserving the most aggressive surgical treatments for the most severe of these combined pancreaticoduodenal injuries. The second is to divert any gastrointestinal secretions to minimize stimulation of the pancreatic exocrine function. The main surgical dictum for treatment of the injuries should be to perform the minimal surgical intervention necessary to adequately treat the injury and accomplish these objectives.
Generic trandate 100 mg with mastercard
This reluctance stems in part from the complexity of liver surgery heart attack heart rate trandate 100 mg with amex, concerns for significant bleeding or gas embolism, and lack of formal training in minimally invasive surgery for the more "senior" hepatobiliary surgeons. However, a dramatic progress in minimally invasive hepatic surgery has been made in recent years. The secondary outcomes include 5-year survival (overall, disease-free, and recurrence-free), resection margins, recurrence pattern, postoperative pain, health-related quality of life, and evaluation of the inflammatory response. Indications and contraindications for laparoscopic liver surgery are shown in Table 125. However, experienced groups have shown that even laparoscopic major hepatectomies can be safely accomplished. Malignant liver tumors, lesions abutting major vasculature, or tumors that are too large to be manipulated laparoscopically should be resected by an open approach. Perihilar cholangiocarcinomas are often challenging even by an open approach, and in general should not be done with a minimally invasive technique. The presence of dense adhesions that prevent safe dissection, unexpected difficulty in manipulating the liver, or failure to make progress are indications for conversion to an open technique. Such a decision is never considered a failure but rather a good judgment call, used to prevent avoidable complications. Reduced postoperative pain, decreased postoperative narcotic requirement, decreased length of hospital stay, lower wound-related complications, and improved cosmesis have transformed minimally invasive liver resection to become the preferred approach when technically feasible. In recent years, minimally invasive major hepatectomy is increasingly performed worldwide, especially at major hepatobiliary centers. More hepatobiliary surgeons are interested in embracing laparoscopic or robotic liver resection in an effort to improve patient results. Herein, we describe outcomes, technical approaches, and current literature relating to minimally invasive hepatic resection. A third option is using the laparoscopic technique for mobilization of the liver before opening the abdomen and completing the resection through a relatively small laparotomy incision (so-called hybrid technique). The benefits of the hand-assisted technique are the relative ease in manipulation of the liver, direct palpation for improved tactile sensation, and the ability for faster control of bleeding in the case of a major vascular injury. Because most specimens mandate a utility incision for intact specimen extraction, the main difference between hand-assisted and pure laparoscopy is the position of the incision. In the operating room the patient is placed in the supine position with both arms extended. The preparation is similar to that of major liver resection, including line placement, bladder catheterization, and orogastric tube insertion. We use a foot board and strapping that allow for steep rotational manipulations of the table during the operation.
Generic trandate 100 mg buy
Nonoperative management of pancreatic injuries has been reported in multiple case series since the 1990s arrhythmia monitoring 100 mg trandate purchase visa. It is an epithelial tumor of low-grade malignant potential, occurring more frequently in females of reproductive age that usually presents as an asymptomatic large mass or with pain. Diagnosis may be made by fine-needle aspirate, which may be accomplished at the time of endoscopic ultrasound in an adolescent patient. A recent review of the National Trauma Database found that nonoperative management of blunt pancreatic trauma in children is a feasible option with equivalent or better outcomes in regard to death, length of stay, Intensive Care Unit length of stay, Intensive Care Unit use, and overall complications. The distal duct presents more straightforward surgical options because a distal pancreatectomy may be accomplished by standard suture or staple closure of the pancreatic remnant without the requirement for an enteric anastomosis. All that may be required is interval drainage of the potentially resulting pseudocyst. Ductal disruption occurred in the midbody in one and in the distal duct in the other, and in one case the stent did not even traverse the injury. Thus the healing of the ductal injury is attributed to decompression of the pancreatic duct as a whole. The investigators pointed out that these cases involved ductal extravasation but not full-scale ductal transection. The remaining three required partial resection or operative treatment of a pseudocyst. Like open operative techniques, these methods rely on the development of a rind around the pseudocyst cavity. Although the success rate was greater than 90%, the authors reported a high complication rate of 33%. Ectopic drainage of the common bile duct into the lesser curvature of the gastric antrum in a newborn with pyloric atresia, annular pancreas and congenital short bowel syndrome. Recurrent pancreatitis caused by pancreatobiliary anomalies in children with annular pancreas. Hyperinsulinism in infancy and childhood: when an insulin level is not always enough. Nesidioblastosis of the pancreas: definition of the syndrome and the management of the severe neonatal hyperinsulinaemic hypoglycaemia. Pancreatic growth and function following surgical treatment of nesidioblastosis in infancy. The changing incidence of acute pan- creatitis in children: a single-institution perspective.
Trandate 100 mg order line
This gradient can be caused by increased resistance to blood flow in the presinusoidal prehypertension warsaw 2014 order discount trandate online, sinusoidal, or postsinusoidal portal circulation. In rare cases, increases in flow in the portal system without concomitant increase in resistance may lead to clinically significant portal hypertension. Portal blood flow is determined by vasoconstriction and dilation of the mesenteric and splanchnic arterioles. In healthy individuals, portal flow is responsible for 75% to 80% of the inflow to the liver, with the remainder coming from the hepatic artery. Total flow ranges from 800 to 1200 mL/min, approximately 25% of total cardiac output. Regulation of hepatic artery flow can compensate for changes in portal venous flow by intrinsic regulatory system known as the hepatic arterial buffer response. The steps in the development of the pathophysiology of portal hypertension have been carefully elucidated in the past two decades in animal models. Portal hypertension is present when portal pressure exceeds 8 mm Hg, but variceal bleeding rarely occurs until portal pressure exceeds 12 mm Hg. However, the inciting event may be one of the other etiologic causes of portal hypertension. This sequence of pathophysiologic changes in the hepatic, splanchnic, and finally systemic circulation offers an opportunity for pharmacologic manipulation and management of portal hypertension. Prehepatic portal hypertension comprises 5% to 10% of portal hypertension patients in the United States and Europe. Prehepatic portal venous obstruction results from thrombosis, invasion by malignant tumor, or constriction from external surrounding processes. Portal and splenic vein thrombosis is the most common cause of prehepatic portal hypertension. Portal vein thrombosis may be associated with umbilical vein catheterization or other causes of sepsis and dehydration in infancy. Other etiologies include pancreatitis and pancreatic tumors, with the later portending a poor prognosis related to the cancer. Prehepatic portal vein thrombosis is typically associated with few downstream signs of liver injury except in preexisting cirrhosis. Finally, hepatic arteryto-portal venous fistulas, usually secondary to a liver biopsy, can occur and if large can lead to portal hypertension. Fistulas are diagnosed with radiologic imaging and can usually be managed with endoluminal angiographic techniques for their occlusion. One important variant of portal hypertensionis leftsided (sinistral) portal hypertension with isolated splenic vein thrombosis, a normal portal vein, and no intrahepatic block.
Lee, 50 years: The short gastric vessels should be preserved, if possible, both to retain their blood supply and to help to anchor the greater curvature. Upper gastrointestinal contrast study in the management of small bowel obstruction-a prospective randomised study. This can then be exchanged for a gentle, noncrushing fine vascular clamp or umbilical tape with a Rumel tourniquet to obtain more secure control. A study from 2015 included 130 resected pancreatic specimens, and the cystic fluid was analyzed by a panel that included mutations in genes, loss of heterozygosity, and aneuploidy.
Sivert, 43 years: Long-term complication following subtotal pancreatectomy for nesidioblastosis: a case report. For patients who undergo cyst fenestration, whether laparoscopic or open, recurrence rates are less than 10%. They may become quite large, get infected, or cause bowel obstruction, and therefore should be excised. Identification of accessory spleens during laparoscopic splenectomy is superior to preoperative computed tomography for detection of accessory spleens.
Arakos, 51 years: Significant long-term pain relief along with weight gain and decreased narcotic dependence are achieved in a majority of patients who undergo operative therapy. Possible signs of mesenteric arterial injury may include bruising to the abdominal wall (seat belt sign), abdominal tenderness, or other signs of peritonitis. Delayed bleeding is one of the most severe postoperative complications after a pancreatectomy. In a multicenter study, radiolabeled intravenous edotreotide induced tumor response or stabilization in 74% of patients with carcinoid tumors that were refractory to octreotide, with a reasonable progression-free survival of 16 months.
Vigo, 57 years: Downstaging of hepatocellular cancer before liver transplant: long-term outcome compared to tumors within Milan criteria. Albumin production serves as a useful marker of liver-specific protein production in support systems using hepatocytes. A prospective study identified a concordance rate of 94% between frozen section and final pathologic examination. The most favorable candidates for therapy are patients with a dominant extrahepatic stricture with or without stones and limited or no intrahepatic involvement.
Volkar, 54 years: Nonenhanced computed tomography image shows a cystic mass containing several daughter cysts (arrows) and peripheral calcification (arrowhead). If a single artery is to be bypassed, saphenous vein or a 6- to 8-mm prosthetic graft is used. Although these tumors often present with similar symptoms, prognosis and treatment depend on the specific type of cancer. The duodenum is divided distal and proximal to the lesion using a stapling device, and the duodenal mesentery and small perforating branches are divided from the head of the pancreas using an energy sealing device.
Hengley, 26 years: M-cells: origin, morphology and role in mucosal immunity and microbial pathogenesis. In addition, there are a host of other disorders that occur in the pediatric population, the most common of which is biliary atresia. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. Necrosis of the tissues results from arterial thrombosis and may necessitate graft removal.
Ilja, 28 years: Occasionally, severe psychiatric or extreme social conditions may also present as relative contraindications. In addition to detection and follow-up of these lesions, imaging is also done to differentiate malignant and nonmalignant cystic lesions, which can be challenging due to the overlapping features of each. The periodic rate of the proximal pacemaker operates at a higher frequency than do pacemaker cells more distally, and thereby override and drive distal pacemaker activity at this higher rate. Pulmonary artery catheterization, or other assessments of central pressure, may be helpful in some cases to guide fluid resuscitation and vasopressor management.
Olivier, 23 years: The response to the decreased blood flow can range from no damage to transmural necrosis. Although all these structures may not be patent in adulthood, vestigial remnants such as fibrous bands will always be encountered by the hand and sight of gifted surgeons. These tests prove only the presence of a fistula and do not identify its site or source. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction.
Tragak, 63 years: An anastomosis of either 29 or 31 mm is desired to promote a good result and less stricturing. Eventually, copper is released from the liver and is deposited in various other organs, including the brain, kidneys, and cornea. In the duodenum, chyme mixes with pancreatic -amylase, which hydrolyzes starches at the interior -1,4 bonds, yielding maltose, maltotriose, and -limit dextrin. This shifts blood flow from the temporarily less important intestinal circulation to the more crucial areas of the heart and brain.
Wenzel, 49 years: These tumor subtypes are further classified by their location, cell of origin, functionality, and specific production of hormones. When the sympathetic system is stimulated, digestive and secretory functions are inhibited. Even prior to frank perforation with gross contamination, there is evidence that bacteria can translocate through the intestinal wall and may well contribute to a deteriorating sepsis picture if the treatment of initial obstruction is delayed. This noninvasive modality has surpassed angiography as the diagnostic modality of choice.
Tizgar, 61 years: There is currently no convincing evidence that high-fiber diets, probiotics, omega-3 polyunsaturated fatty acids, glutamine supplementation, or antioxidants affect the disease course of patients with Crohn disease. Recurrence and survival after resection of small intraductal papillary mucinous neoplasm-associated carcinomas (20-mm invasive component): a multi-institutional analysis. The biliary limb includes the length of the duodenum and approximately 30 cm of jejunum measured from the ligament of Treitz. Without ileal reabsorption, hepatic synthesis of bile salts would not be sufficient for fat digestion.
Fadi, 38 years: Other: this category includes vagal injury during the previous procedure resulting in poor gastric emptying as well as esophageal dysmotility. As the name implies, nonocclusive mesenteric ischemia does not require a fixed defect to be present for acute ischemia to develop. Interestingly, even within the cohort of patients who underwent complete R0 resection, the performance of partial hepatectomy conferred a statistically significant survival advantage on multivariate analysis. Reconstruction is performed in a similar fashion to the open technique, consisting of an end-to-side, duct to mucosa, 1- or 2-layer pancreaticojejunostomy, a single layer end-to-side hepaticojejunostomy, and an end-to-side, antecolic duodenojejunostomy.
Ressel, 39 years: Bentrem, Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, Illinois. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Sepsis control and correction of postoperative infection is critical to preventing ileus and early intestinal atrophy. The majority of patients with chronic radiation enteritis require an operation for intestinal obstruction.
Silas, 41 years: The effect of N-acetylcysteine on oxygen transport and uptake in patients with fulminant hepatic failure. Initial efforts should be directed toward intravenous fluid resuscitation, control of infection, ongoing measurement of fistula and urine output, and protection of the surrounding skin. Evaluation of the International Study Group of Pancreatic Surgery definition of post-pancreatectomy hemorrhage in a high-volume center. There is a lack of consensus on the surgical treatment of metastatic tumors to the pancreas.
Emet, 29 years: Attempts at repair by the primary surgeon were successful only in 17% of cases, and in no case was a secondary repair by the primary surgeon successful. As such, the debate about the optimal management of patients with choledocholithiasis has persisted for many years. The swinging pendulum: a national perspective of nonoperative management in severe blunt liver injury. When detected, it may be addressed with endovascular techniques, including percutaneous transluminal angioplasty or primary stent placement, avoiding the dire complications of thrombosis.
Tom, 35 years: A wide Kocher maneuver is performed, and the jejunum is divided with a stapler 10 cm from the ligament of Treitz. The lesion may show a "mosaic" appearance because of combined areas of growth and necrosis. One-step palliative treatment method for obstructive jaundice caused by unresectable malignancies by percutaneous transhepatic insertion of an expandable metallic stent. This final anastomosis is generally stapled, although a sewn 2-layer anastomosis is acceptable.
Tarok, 65 years: Lethal toxicity may occur due to depletion of the large progenitor population, not the stem cell population, which is considered radioresistant possibly due to high levels of antioxidants. Vasculobiliary injuries may also have specific effects on the arteries (pseudoaneurysm with delayed hemorrhage), bile ducts (necrosis, stenosis, cholangitis), and/or liver (necrosis, atrophy) over variable lengths of time. The cisterna chyli is located below the level of the diaphragm at the end of the thoracic duct anterior to the lumbar spine and posterior to the aorta. Significant long-term survival after radiofrequency ablation of unresectable hepatocellular carcinoma in patients with cirrhosis.
10 of 10 - Review by D. Cobryn
Votes: 312 votes
Total customer reviews: 312