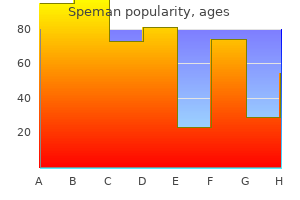
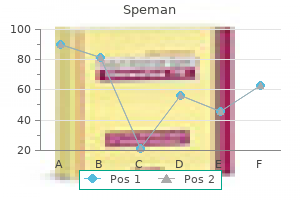
Speman
Speman dosages: 60 pills
Speman packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles
60 pills speman with amex
The interest in liver-assist devices is great prostate cancer ketoconazole discount speman 60 pills without prescription, due to high mortality rates, increasing wait lists, an expansion of indications for transplantation, and major liver resections. This article emphasizes novel and promising techniques, such as extracorporeal liver support, cell transplantation, and tissue engineering. A historic summary of the different attempts to support the failing liver is also reviewed. The goals of medical therapy are to (1) facilitate recovery, (2) reduce ongoing liver injury. Vitamin K is administered to prevent or correct coagulopathy (Pereira et al, 2005). Lactulose is given orally or rectally with the goal of at least two loose stools per day. Nutritional support is initiated (either enteral or parenteral, depending upon the clinical picture) with a protein load not to exceed 0. Branched-chain amino acids (HepatAmine) are used at the discretion of the dietitian. If these patients require sedation, we advocate the use of the short-acting agent propofol (Wijdicks et al, 2002). Goals of ventilator support are to maintain a partial pressure of oxygen in arterial blood (PaO2) higher than 70 mm Hg, preferably by using a fraction of inspired oxygen (FiO2) of less than 40%. Intravenous fluids are adjusted to maintain serum sodium between 145 to 155 mEq/L. Ultrasound evaluation to assess hepatic vasculature and exclude mass lesion is obtained. Hemodynamic instability may occur at this stage secondary to a systemic inflammatory response (Rolando et al, 2000) or intravascular depletion. Some institutions discontinue hypothermia before transplant due to risk of bleeding, whereas other centers continue hypothermia until 24 hours after liver transplant because of late risks of cerebral edema. If seizures occur in these patients, metabolic causes such as hypoglycemia and electrolyte imbalances must be ruled out. Phenytoin should be administered to control seizures, and short-acting benzodiazepines can be used in phenytoin-refractory cases. Electroencephalographic monitoring is initiated in the case of status epilepticus, which is treated with benzodiazepines. The results of early clinical trials were discouraging; encephalopathy often improved temporarily, but patient survival was not affected. In addition, a significant complication rate was reported with plasma exchange, including chemical toxicity, viral infections, and death from lung and brain complications (Brunner et al, 1987). Of the patients with acetaminophen intoxication, 25% died, and 21% were bridged to transplantation. In this Japanese study, all patients regained consciousness, and brain edema or hepatorenal syndrome did not develop in any patient during plasma exchange and hemodiafiltration treatment.
Order speman 60 pills with amex
Fiamingo P androgen hormone youtube discount speman 60 pills buy online, et al: Incidental cystadenoma after laparoscopic treatment of hepatic cysts: which strategy Fukunaga N, et al: Hepatobiliary cystadenoma exhibiting morphologic changes from simple hepatic cyst shown by 11-year follow up imagings, World J Surg Oncol 6:129, 2008.
Syndromes
- Eat sweets that are sugar-free.
- If the medication was prescribed for the patient
- Unsteadiness
- Milk
- Finishing your antibiotics when you are treated
- Budd-Chiari syndrome
Purchase generic speman
When present prostate cancer and diet 60 pills speman buy visa, macroaneurisms (large central vessels) within the lesions are highly characteristic. Liver biopsy is mandatory for most patients with angiomyolipomas, and histologic diagnosis is based on the identification of the different components. Histologic diagnosis might be challenging in patients with lesions that have prominent proliferation of epithelioid cells and a scarcity of adipose tissue. When a diagnosis for angiomyolipoma is established, careful observation with serial imaging follow-up is recommended in asymptomatic patients who have lesions less than 5 cm in diameter (Sawai et al, 1998). As a matter of fact, these lesions have the highest risk of malignant transformation, especially when major epithelioid content is present. Even though arterial embolization is now often considered as first-line treatment for kidney angiomyolipoma with good results (Faddegon & So, 2011; Ramon et al, 2009), the lack of reported experience of using arterial embolization for treating hepatic angiomyolipoma renders the benefits of this potentially valuable therapy merely speculative. Biliary Hamartoma these lesions are also known as the Von Meyenburg complex and usually present as multiple and small (<5 mm) nodules scattered throughout the liver (see Chapter 89). Their prevalence in adults is approximately 5% in autopsy series, and they are particularly frequent in patients with congenital hepatic fibrosis or polycystic liver disease (Redston & Wanless, 1996). Biliary hamartomas comprise abnormal development of small intrahepatic bile ducts and are composed of bile ductules, inflammatory cells, and fibrosis (see Table 90A. The main practical problem raised by this tumor is for the pathologist because its possible discovery during surgery for carcinoma of another abdominal organ leads the surgeon to perform a biopsy for frozen-section diagnosis (Guiu et al, 2009). The pathologist who is unaware of this rare entity may be puzzled and tempted to call the lesion metastatic carcinoma. Bile Duct Adenoma Bile duct adenoma, also called benign cholangioma, is a benign and asymptomatic lesion that is typically discovered incidentally in imaging studies, surgery, or at autopsy (Kim et al, 2010). Bile duct adenomas are usually small in size (<5 mm), well circumscribed, and subcapsular (see Chapter 89). These lesions comprise the proliferation of noncystic biliary structures within a dense fibrous stroma (Allaire et al, 1988). The overlapping histologic features with biliary hamartomas have led some authors sometimes to consider bile duct adenomas as a variant of biliary hamartomas. This finding has also led some authors to support an "adenoma to Lipoma Hepatic lipoma is a very rare liver tumor that can mimic angiomyolipoma (see Chapter 89). Hence resection was not justified, and the only clinical significance of these lesions was in the possible confusion with metastatic carcinoma during surgery (Hornick et al, 2005). Whether the identification of oncogenic mutations should lead to changing the current nonaggressive policy regarding these lesions remains to be assessed. Commonly found in the lung, inflammatory psuedotumors are considered to be a result of an exaggerated inflammatory response, often associated with various inflammatory diseases (Faraj et al, 2011).
Buy genuine speman on-line
Complications were seen in 15% mens health questionnaire speman 60 pills without prescription, and one patient died of a pancreatic abscess after a failed cannulation. Of concern, 50% of patients evaluated at the time of stent removal had stentinduced dorsal duct changes. Ten patients were randomized to stent placement, and nine were randomized to no treatment, with follow-up for 1 year. In the stent group, no patients subsequently came to the hospital with pain, but five patients in the control group were admitted, and two more came in with pain. Furthermore, nine patients in the stent group rated their pain improved by 50% or more, but only one patient in the control group reported a similar improvement. It has been pointed out that a significant period of time can exist between attacks of pancreatitis in this patient group, and this study has since been criticized on the basis of the short duration of follow-up. Follow-up data were available for 113 patients (78%), and the median follow-up time was 43 months. The majority of patients had a needle-knife sphincterotomy (82%) and temporary stent placement (90%). In a multivariate analysis that corrected for age, gender, symptom frequency/duration, and length of follow-up, chronic pancreatitis and younger age both independently predicted failure of improvement after treatment. In the largest published series by Warshaw and colleagues (1990), 88 patients with recurrent acute pancreatitis (49%) or "pancreatic pain" (51%) had minor papilla sphincteroplasty with a mean follow-up of 53 months; 70% of patients were reported to show improvement, 85% if the minor papilla was stenotic at surgery, compared with 27% if it was not (P <. Of those with recurrent acute pancreatitis, 82% were reported to have improved compared with 56% in the chronic pain group (P <. Seven patients were documented to have developed a restenosis at the minor papilla, six of whom had further surgery. In a study by Pappas and colleagues (2013), 14 patients (6 pancreas divisum, 5 alcohol, and 3 idiopathic) who underwent the Frey procedure for chronic pancreatitis and disease-related intractable pain were compared. The authors commented on the potential advantage of this approach over minor duct sphincteroplasty and lateral pancreaticojejunostomy in the removal of the fibrotic tissue of the head of the pancreas, the potential origin of the pain. Patients in groups used as controls often only have cholangiography and do not undergo intentional pancreatography. Cystic Fibrosis and Recurrent Pancreatitis Cohn and colleagues (1998) and Sharer and colleagues (1998) first described the link between cystic fibrosis gene mutations and idiopathic pancreatitis (see Chapters 4 and 57). Includes patients graded excellent, good, and fair (if more than 50% improved and off narcotics). Pain suggestive of pancreatic origin (generally epigastric with back radiation) without serologic, ultrasound, computed tomographic scan, or ductographic evidence of pancreatitis. At best, careful case selection is paramount before embarking on any such therapy. Patients most likely to benefit are older, have documented recurrent acute pancreatitis, and have been thoroughly investigated for a recognized cause of pancreatitis. Those with chronic pancreatitis or pancreas-type pain are much less likely to benefit. Recurrence of symptoms is common, and repeat therapy involving the minor ampulla may be required.
Buy speman 60 pills fast delivery
Lymphocytes and histiocytes also may be present (Colombat et al man health trend order discount speman, 2002), sometimes in the form of lipogranulomas, and megamitochondria also may be evident. In the portal and periportal regions, ductular reaction with numerous neutrophils may occur. Cholangiolitis and canalicular bile plugs are worrisome lesions for concomitant pancreatitis. Fibrosis usually involves the terminal hepatic venules, leading to the thickening of the wall; luminal occlusion may be seen with necrosis of adjacent hepatocytes and Mallory-Denk bodies within remaining hepatocytes, a lesion referred to as central hyaline necrosis. Subendothelial fibrosis is a venoocclusive lesion of alcoholism that may be noted even in end-stage cirrhotic livers. Fibrosis may extend into the lobules in perisinusoidal spaces as delicate or dense strands, giving rise to a distinctive "chicken wire" pericellular (perisinusoidal) distribution. The liver may shrink and be nearly replaced by fibrosis, and the cirrhosis may evolve into a macronodular or mixed nodular architecture with characteristic broad septa. Steatosis, ballooning, and Mallory-Denk bodies may not be discernible, especially in patients who have stopped consuming alcohol for several months or years. The lesions noted in liver tissue may resemble many of the features of alcohol-induced liver damage in individuals who are not heavy drinkers (Brunt et al, 2012). The disease is etiologically attributed primarily to insulin resistance and is considered the hepatic manifestation of the metabolic syndrome, a constellation of risk factors for cardiovascular disease that includes obesity, hypertension, diabetes, and hyperlipidemia (Marchesini et al, 2001) (see Chapter 71). Recently, an immunohistochemical stain to detect loss of K8/18 in ballooning, as well as presence of clumped K8/18 in Mallory-Denk bodies, has been introduced (Lackner et al, 2008). If numerous MalloryDenk bodies are present in the background of steatohepatitis, an alcoholic origin is more likely (Brunt et al, 2012). Zone 3 "chicken wire" perisinusoidal fibrosis; this feature can be seen in nonalcoholic and alcoholic steatohepatitis (Massontrichromestain). This typically does not obliterate the terminal hepatic venules, a feature dissimilar to alcoholic hepatitis. Similar to the widespread use of grading and staging in other forms of chronic liver disease, this proposal was made in recognition of the unique features of steatohepatitis to facilitate further reproducible evaluation for clinical and laboratory investigation. Confluent or multiacinar bridging necrosis with collapse of the lobular framework may be seen. However, changes resembling ground-glass inclusions have been observed in a variety of conditions (Wisell et al, 2006). A definitive diagnosis can be established by histochemical stains (orcein, Victoria blue) or with immunohistochemical detection of hepatitis B surface antigen in the cytoplasm and hepatitis B core antigen in the nucleus. Interestingly, even after virologic cure, a small number of individuals from large clinical trials (7% to 13%) continue to have fibrosis progression or even cirrhosis.
Quality 60 pills speman
Externalviewofasuperficial tumor bulging under the capsula prostate urinary problems generic 60 pills speman mastercard, with large subcapsular and dilated vessels. Soft,well-delineatedtumor with little or no fibrous capsule and small heterogeneous foci of hemorrhage. Cellular atypias can be impressive, especially in patients who have taken steroids for many years. Vascular changes, including sinusoidal dilation, peliosis, infarcts, and hemorrhage are frequent. These changes may leave edematous or fibrotic regions, often with hemosiderin-laden macrophages. Nevertheless, these tumors share the same clinical and imaging characteristics independently of their number (Dokmak et al, 2009; Lewin et al, 2006). The three main morphologic patterns of liver adenomatosis have been described: the steatotic form, the peliotic/telangiectatic form, and the mixed form (Lewin et al, 2006). Histologically, the hepatocellular proliferation contains small clusters of arteries embedded in collagen, often associated with an inflammatory infiltrate (lymphocytes and macrophages) and occasionally ductular proliferation. In addition, foci of sinusoidal dilation and peliotic changes are usually present. It is the second most frequent primary malignant tumor of the liver (5% to 15% of liver primary malignancies) (Malhi et al, 2006; Welzel et al, 2006). Hepatholithiasis (see Chapter 39), cholelithiasis (see Chapter 32), cholangitis (see Chapter 43), chronic pancreatitis (see Chapter 57), and exposure to Thorotrast are also risk factors (Chapman, 1999; Kim et al, 2015; Lipshutz et al, 2002). In the intraductal growth type, tumor often spreads intraluminally along the ducts. Bloodborne spread occurs later, particularly to the lungs (Jiang et al, 2009; Patel, 2001; Suzuki et al, 2002). These patterns are associated with different clinical evolutions, with intraductal growth and the periductal infiltration showing the best and worst prognosis, respectively (65% survival at 5 years compared with less than 5% at 5 years) (Jiang et al, 2009; Rizvi et al, 2014; Suzuki et al, 2002). In case of large tumors, adjacent satellite tumoral nodules are commonly observed. The pure periductal-infiltrating type and the intraductal growth pattern are seldom observed (Guglielmi et al, 2009). Cytoplasm is usually pale, slightly eosinophilic, and sometimes more abundant and clear. Mucus secretion may be highlighted by alcian blue staining, although the amount is usually small. Less differentiated tumors may show cribriform formations and/or a cordlike pattern, and poorly differentiated cancers are characterized by marked cellular pleomorphism.
Apium crispum (Parsley). Speman.
- What is Parsley?
- How does Parsley work?
- Are there any interactions with medications?
- Are there safety concerns?
- Dosing considerations for Parsley.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96771
Speman 60 pills buy fast delivery
Patients typically are seen for medical attention after the development of jaundice secondary to biliary obstruction prostate 049 buy speman 60 pills line, and optimal patient management requires thorough workup and multidisciplinary evaluation for the proper selection of patients who may be eligible for resection. In this article we review the etiology, workup, and staging of primary tumors of the extrahepatic biliary tree, specifically biliary adenocarcinoma or cholangiocarcinoma, and discuss surgical and nonsurgical options for treatment of patients with this challenging disease process. In total, cholangiocarcinomas account for 3% of gastrointestinal malignancies (De Jong et al, 2012), with an annual population incidence in the West of 0. This incidence varies with geography, and in some parts of Asia the incidence can be as high as 113 per 100,000 for males and 50 per 100,000 for females (Tyson & El-Serag, 2011). In the United States, approximately 5000 new cases of cholangiocarcinoma occur yearly (De Jong et al, 2012). Anatomically, cholangiocarcinoma is categorized as either intrahepatic or extrahepatic based on their location. In the United States, approximately 3000 new cases of extrahepatic cholangiocarcinoma occur yearly (Siegel et al, 2015), with the majority arising from the biliary confluence (hilar cholangiocarcinoma). Hilar cholangiocarcinoma was originally described by Klatskin in 1965, and these malignancies account for approximately 50% of all cholangiocarcinomas (De Oliveira et al, 2007). The majority of these malignancies develop sporadically, but certain risk factors for their development exist. Another risk factor for cholangiocarcinoma is biliary cystic disease, also known as choledochal cysts, which are congenital dilations of the biliary tree (see Chapter 46). The lifetime risk of cholangiocarcinoma in patients with choledochal cysts is 818 estimated to range from 6% to 30% (Suarez-Munoz et al, 2013), and cholangiocarcinoma develops in these choledochal cyst patients earlier, with a mean age of 32 at diagnosis of malignancy in one series (Valero et al, 2012). Resection of the extrahepatic biliary tree before development of cancer and reconstruction by Roux-en-Y hepaticojejunostomy can lead to overall survival of as much as 96% (Ono et al, 2010). Even after resection of choledochal cysts, however, these patients are at risk for the late development of cholangiocarcinoma and require long-term surveillance (Soares et al, 2014). Parasitic infections of the bile ducts are also risk factors for cholangiocarcinoma (see Chapter 45). Increased risk is seen in infections from liver flukes (Clonorchis sinensis and Opisthorchis viverrini), which lay eggs in the biliary tree, resulting in chronic inflammation and presumed malignant transformation of the biliary epithelium (Watanapa, 1996; Watanapa & Watanapa, 2002). Infections from biliary ascariasis or hepatic schistosomiasis are also risk factors for the development of cholangiocarcinoma (Cai et al, 2011). Chronic hepatolithiasis is a risk factor for cholangiocarcinoma, which again is presumed to arise in the setting of chronic inflammation of the bile ducts and biliary stasis (see Chapters 39 and 44).
60 pills speman buy with mastercard
Once a decision is made that intervention is required man health 2014 report trusted 60 pills speman, these poorly demarcated pancreatic (and peripancreatic) collections can be managed by a variety of approaches. Freeny and his colleagues (1998), in the 1990s, showed that aggressive percutaneous sepsis control would promote recovery in the absence of formal necrosectomy, although a number required subsequent surgical intervention. Laparoscopic direct necrosectomy was described in the 1990s but failed to gain popularity due to technical difficulty (Gagner, 1996). There are only two recent retrospective studies (Parekh, 2006; Zhu et al, 2001) describing laparoscopic necrosectomy alone, in a total of 29 patients. The patients were highly selected, and no median follow-up was available for either study (Parekh, 2006; Zhu et al, 2001). Connor and colleagues (2005) reported half as many deaths in patients treated with a minimal access approach when compared with those having laparotomy. Patients with infected pancreatic necrosis were randomized to either open necrosectomy or a step-up approach based on endoscopic or percutaneous drainage as the initial intervention, with progression to retroperitoneal debridement with lavage if no improvement was observed. The composite end point of death or major complication demonstrated a significant benefit with the step-up approach. Indeed, 35% were successfully managed with percutaneous drainage alone and did not require subsequent debridement. There is now a consensus advocating a principle of early organ support and nutritional optimization, followed ideally by delayed minimally B. The choice of one approach over another is determined by the clinical condition of the patient, local experience and expertise, anatomic position/content of the collection, and the time from presentation/maturation of the wall of the collection. There is an acceptance that due to the complexity of presentation, no single technique is applicable in all circumstances. The choice of initial percutaneous or endoscopic drainage is now largely based on the position of the collection relative to the stomach, colon, liver, spleen, and kidney. In general, our practice has been to approach lateral collections and those extending behind the colon from the left or right flank and to prefer endoscopic drainage for those medial collections where a percutaneous route is compromised by overlying bowel, spleen, or liver. The route of percutaneous drainage should ideally take into account the probability of subsequent step-up escalation, siting the drain as lateral and inferior as possible and avoiding the costal margin. If the initial drain placement is suboptimal, secondary alternative access can be obtained, sometimes involving a combination of percutaneous and endoscopic techniques. This open approach was associated with major morbidity (enteric fistula, 45%; hemorrhage, 40%; and colonic necrosis, 15%), and failed to gain popularity. For both minimally invasive techniques, a left-sided small-diameter percutaneous drain is ideally placed into the acute necrotic collection between the spleen, kidney, and colon. In those who fail to respond adequately to simple drainage, this access drain is then used as a guide to gain enhanced drainage of the collection.
Order speman 60 pills on-line
There is a high incidence of rebleeding once the tube is removed and therefore should only be use as a temporarily measure to a more definitive treatment prostate jaculation speman 60 pills purchase line. A Emergency Surgical Approaches and Emergency Portosystemic Shunts B Emergency creation of portosystemic shunts or other surgical therapy is usually a last resort for persistent, acute, exsanguinating variceal hemorrhage (see Chapters 84 to 87). Patients with shunts who come to the emergency department often have gastric variceal bleeding. It has been used effectively in critically ill adults to control bleeding before liver transplantation, and it has also been used in some children with bleeding stomal varices (Lagier et al, 1994). The procedure appears to decrease portal pressure acutely, although complications include risk for shunt occlusion and increase encephalophathy; therefore it is best viewed as a bridging procedure only. Pediatric application is limited by size constraints, but in experienced hands and in selected children older than 2 to 5 years, the procedure has application and is preferable to major shunt surgery for hepatic causes of portal hypertension. Ablation of esophageal varices by sclerotherapy in a 6-year-old child with portal hypertension after a Fontan procedure for congenital heart disease. When the patient is hemodynamically stable, endoscopy treatment is indicated for an acute esophageal variceal bleeding. It is important to document the source of the bleed because a significant percentage of patients with known varices have bleeding from sources other than varices, including duodenal or gastric ulceration. Both techniques are well described in children (Goenka et al, 1993; Goncalves et al, 2000; Zargar et al, 2002). In adults, comparative trials of sclerotherapy and ligation indicate equal efficacy in controlling bleeding, reducing rebleeding, and ablating varices, but fewer adverse effects are reported with banding. Banding is the recommended endoscoping treatment option, but ligation may be technically difficult in an esophagus awash with blood or for small varices, particularly in small infants, where entrapment of part of the esophageal wall with perforation or bleeding can occur (Banares et al, 2002). Sclerotherapy involves injection of sclerosant (ethanolamine or tetradecyl sulfate), either paravariceally or intravariceally in volumes of 0. Care should be taken to avoid injecting too high above the cardia, which can increase bleeding from a distal varix. This procedure can be associated with bacteremia, and broadspectrum antibiotics should be prescribed (amoxicillin, cefuroxime, metronidazole). Complications, which should be uncommon in experienced centers, include esophageal ulceration, stricture, and pain. In adults, nonselective -blockers, such as propranolol, reduce hepatic arterial and portal vein blood flow and have been studied with respect to reduction in portal pressures to less than 12 mm Hg, thereby reducing the risk of an initial hemorrhage (Shasidhar et al, 1999) and are recommended for the prevention of first variceal hemorrhage. However, in children, there is still uncertainty regarding efficacy and safety about the use of these pharmacologic agents. Under certain circumstances, prophylactic sclerotherapy or banding may be indicated, but the potential in children for bleeding of known varices that have never bled is conjectural.
Discount speman 60 pills on-line
Alternatively androgen hormone 24 speman 60 pills buy overnight delivery, when the left side of the liver is functional, a left drainage can be performed as the next step; then one stent can be placed from the left, and another can be placed from the right. Although a significant difference in patency is reported when more than one stent is placed in a noncoaxial manner (Maybody et al, 2009), the mean patency of multiple stents is almost 6 months, justifying stent placement. Even when one part of the liver is not functional, drainage may be necessary to eliminate a source of ongoing cholangitis. The concepts of biliary drainage are simple, but when high bile duct obstruction is present, the planning is complex, and execution can be difficult. The patient must have enough of the liver drained to be free of cholangitis and pruritus and to effect a reduction in serum bilirubin to receive chemotherapy, if indicated. Given that no difference in stent patency is reported if the stent is inserted for proximal or distal obstruction, that a significant difference in patency is seen when more than one stent is placed, and that lower complication rates are reported when stents are placed primarily, primary stent placement should be considered whenever possible (Inal et al, 2003a, 2003c; Maybody et al, 2009). With proper technique, including peripheral bile duct puncture, serious bleeding complications are uncommon. Because the hepatic artery, portal vein, and bile duct travel side by side within portal triads, blood may enter the bile duct during catheter exchanges, resulting in hemobilia in the immediate postprocedure period (see Chapter 125). Hemobilia usually clears within 24 hours, and new or recurrent hemobilia within the first few days of drainage typically is related to catheter malposition. If the catheter is pulled out from its original position, a catheter sidehole may become positioned adjacent to a portal vein branch; this problem can be corrected by simply repositioning the catheter, but the catheter is often upsized as well. No matter where the initial puncture is performed to opacify the biliary tree, attempts are always made to puncture a peripheral bile duct for catheter placement, preferably a fourth-order or fifth-order branch. The more peripheral the bile duct punctured, the smaller the accompanying hepatic artery branch, and the lower the risk of arterial injury and postprocedure bleeding. When bleeding occurs 1 week or more after biliary drainage- especially when the event is sudden in onset, and there is not only hemobilia but bleeding around the catheter entry site-arterial injury should be suspected, and the patient should be studied angiographically. If the operator is determined to demonstrate extravasation of contrast material angiographically, it is sometimes necessary to remove the biliary drainage catheter over a guidewire during the angiogram. Despite prophylactic antibiotic coverage, sepsis may occur immediately after or within several hours of drainage and should be treated appropriately (Smith et al, 2004). This is most frequently manifested by the development of rigors with normal or low body temperature, but hypotension and fever may also occur. Sepsis is managed with continued administration of appropriate antibiotics, expansion of intravascular volume, and pressor support if necessary. Blood cultures should be drawn to identify organisms responsible for the bacteremia. This is particularly important for those with preprocedure fever, biliary-enteric anastomosis or sphincterotomy, previous endoscopic retrograde cholangiopancreatography, or an indwelling stent or catheter. Although positive bile cultures are more common in patients with benign bile duct obstruction, cultures are positive in more than half of patients with malignant obstruction.
Marus, 42 years: A similar study by Ferrone and colleagues (2008) revealed an actual 5-year survival rate of 23% for resected stage Ia disease, and all-stage actual 5 year and 10 year survival rates of 12% and 5%, respectively, were reported. Chronic pancreatitis may be associated with epithelial atypia, both architectural and cytologic; conversely, ductal adenocarcinoma is notorious for its deceptively bland appearance. The history of the definition and classification of pancreatitis shows the progressive awareness of experts that acute and chronic inflammation should be defined by different pathologic, clinical, and etiogenetic perspectives (Table 54. The concept of the Sugiura procedure seemed to be more universally accepted of the two approaches.
Finley, 60 years: Fragmentation of the specimen noted at the time of biopsy should raise the suspicion of cirrhosis. Campbell F, et al: Classification of R1 resections for pancreatic cancer: the prognostic relevance of tumour involvement within 1 mm of a resection margin, Histopathology 55(3):277283, 2009. The ischemic jejunal limb is then rotated under the ligament of Treitz to the right upper quadrant. The relatively few side effects seen with the recently approved agents have done away with many of these concerns.
Achmed, 27 years: Tahvanainen P, et al: Polycystic liver disease is genetically heterogeneous: clinical and linkage studies in eight Finnish families, J Hepatol 38:3943, 2003. Hytiroglou P, et al: Hepatic precancerous lesions and small hepatocellular carcinoma, Gastroenterol Clin North Am 36:867887, 2007. Porta M, et al: Serum concentrations of organochlorine compounds and K-ras mutations in exocrine pancreatic cancer, Lancet 354:2125 2129, 1999. Specific serologic tests are available that can be used to monitor successful treatment (Santra et al, 2001) but are not commonly used in clinical practice.
Ateras, 45 years: This technique is simple and useful in patients with locally advanced perihilar cholangiocarcinoma that requires combined hepatic artery and portal vein resection, in whom hilar dissection cannot be completed before liver resection. Igami T, et al: Surgical treatment of hilar cholangiocarcinoma in the "new era": the Nagoya University experience, J Hepatobiliary Pancreat Sci 17(4):449454, 2010. The diagnosis is made on the basis of a temporal relationship between exposure to the drug and the development of acute liver failure and the more common offending drugs are listed in Box 79. Schramek A, et al: New observations in the clinical spectrum of the Budd-Chiari syndrome, Ann Surg 180:368372, 1974.
Yugul, 55 years: Pseudocysts can be managed with observation, endoscopic drainage, or operative drainage (Cannon et al, 2009). Metronidazole reaches high concentrations in the liver and intestine, and it crosses the placenta and the blood-brain barrier. Kloppel G, et al: Precancerous lesions of the biliary tree, Best Pract Res Clin Gastroenterol 27(2):285297, 2013. Based on the cell of origin, the most frequent solid benign tumors may be classified into two groups according to their epithelial or mesenchymal origins.
Sibur-Narad, 46 years: However, these structures can be mistaken for septa within the abscess cavity, and fracturing of these strands can lead to hemorrhage or biliary leak, or it can create a communication between the vascular and biliary channels and result in hemobilia and jaundice (Singh et al, 2008). Recent studies have suggested that coffee intake reduces the risk (Bamia et al, 2014; Bravi et al, 2013). Cytoreductive surgery that reduces disease to less than 1 cm when combined with chemotherapy is an accepted treatment approach. Otto G, et al: Klatskin tumour: meticulous preoperative work-up and resection rate, Z Gastroenterol 49(4):436442, 2011.
Daryl, 57 years: In children, common causes include forms of infant cholestasis, such as biliary atresia, as well as a range of metabolic disorders, infections, toxins, and vascular and nutritional diseases. In common practice, the antibiotics of choice are third-generation cephalosporins. Endoscopically, in the second portion of the duodenum, proximal to the ampulla, mucosal nodularity is present that microscopically reveals inflamed mucosa, Brunner gland hyperplasia, or a myoid spindle cell proliferation in the submucosa that can also extend to the mucosa. When patients cannot be palliated in this fashion, surgical palliation through gastrojejunostomy and Roux-en-Y hepaticojejunostomy (see Chapter 31) is indicated to relieve symptoms of duodenal and biliary obstruction, respectively, and to allow physiologic improvement such that patients can subsequently receive palliative chemotherapy or chemoradiotherapy.
Cruz, 47 years: Prolonged fever with no obvious cause is observed in 10% of patients (see Chapter 27). An umbrella-shaped laparoscopic trocar for evacuation of the cysts has been used with a locking mechanism that enables the surgeon to suspend the cyst wall against the abdominal wall (Seven et al, 2000). The presence and extent of nodal metastatic disease are important prognostic factors. Different cell types can be observed intimately admixed in the transitional region.
Redge, 35 years: For these reasons, pure drainage procedures have been replaced by techniques that combine resection and drainage for the majority of patients. Orozco H, et al: Is splenectomy necessary in devascularization procedures for treatment of bleeding portal hypertension The latter may be associated with bacterial translocation, bacteremia, and ultimately, infected pancreatic necrosis. A variety of pancreatic neoplasms can show prominent intraductal growth, including acinar cell carcinomas (Ban et al, 2010; Basturk et al, 2007), pancreatic neuroendocrine tumors, osteoclastic giant cell carcinomas (Muraki et al, 2016), and even metastatic tumors, and thus fall into the differential diagnosis of these intraductal neoplasms.
Xardas, 62 years: It can be associated with serious morbidity and mortality and may cause anemia, chronic pain, diarrhea, exercise intolerance, malnutrition, bladder cancer, portal hypertension, and central nervous system complications (King et al, 2005). Helmy A, et al: Updates in the pathogenesis, diagnosis and management of ectopic varices, Hepatol Int 2(3):322334, 2008. Five days of therapy are as efficacious as 10 days of therapy (Runyon et al, 1991). The dose is doubled in a coordinated fashion with increases in spironolactone until therapeutic effect is achieved.
Shakyor, 28 years: Adequate drainage of the pancreatic tail has to be verified by probing of the duct. Signs of hepatic encephalopathy are subtle and uncommon in children with portal hypertension. It is important to assess the relationship of the cyst to the inferior vena cava, hepatic veins, and porta hepatis structures because large or multiple cysts frequently distort normal liver anatomy. The high concentration of albumin is believed to facilitate removal of nonpolar molecules known to bind to albumin.
Pyran, 63 years: In this setting, a two-step operative strategy with portal vein occlusion might be required. Even with massive organ enlargement, significant hepatic complications remain fairly uncommon, although patients (or others) may have noted a protuberant abdomen. In developed countries, it continues to be encountered sporadically in immigrants or travelers from endemic zones, low socioeconomic groups, residents of institutions, and male homosexuals (Ravdin & Stauffer, 2005). Primary end points were survival probabilities at days 28 and 90, irrespective of liver transplantation.
Konrad, 59 years: The liver is commonly small and impalpable; with an intrahepatic cause; however, it can be enlarged, hard, or nodular with a small right lobe and/ or splenomegaly. A favorable response in reduction of serum tumor markers following ablation may predict the durability of symptomatic response and may be associated with improved survival and decreased incidence of disease progression (Berber et al, 2002). Endoscopic and minimally invasive techniques have the advantage of reduced morbidity over open surgery (Zhi et al, 2004). This study, combined with the data from Sakamoto and colleagues (2006), reinforces that stage of disease, not extent of surgery (assuming an R0 resection), determines survival in patients who undergo resection of gallbladder cancer.
Bufford, 50 years: Watanapa P: Cholangiocarcinoma in patients with opisthorchiasis, Br J Surg 83:10621064, 1996. Portal hypertension can arise from cirrhotic and noncirrhotic causes, although as a manifestation of portal hypertension, ascites is most common in disorders that increase pressures within the hepatic sinusoids, either from sinusoidal (cirrhosis) or postsinusoidal processes (heart failure, hepatic venous obstruction). Sakamoto Y, et al: Clinical significance of extrahepatic bile duct resection for advanced gallbladder cancer, J Surg Oncol 94(4):298306, 2006. Genotype 4 is occasionally seen in the United States, although is more commonly seen in the Middle East and northern and central Africa.
Mine-Boss, 58 years: On immunohistochemistry, the tumors strongly express the general neuroendocrine markers chromogranin and synaptophysin, and most express keratin as well (Albores-Saavedra et al, 2015; Burke et al, 1989). The point where the cyst is to be entered is identified, and the smallest possible working area is delineated by additional packing. Patients with locally advanced gallbladder tumors should be evaluated carefully to rule out distant metastases. Okuda H, et al: Epidemiological and clinical features of Budd-Chiari syndrome in Japan, J Hepatol 22:19, 1995.
9 of 10 - Review by I. Grompel
Votes: 310 votes
Total customer reviews: 310