Calcitriol
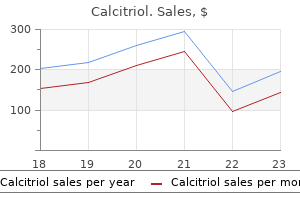
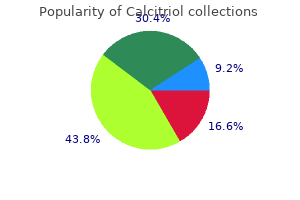
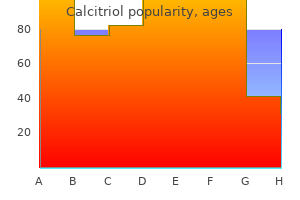
Calcitriol dosages: 0.25 mcg
Calcitriol packs: 30 caps, 60 caps, 90 caps, 120 caps, 180 caps, 270 caps, 360 caps

0.25 mcg calcitriol buy visa
The accrual goal in this trial was 800 patients; however treatment genital herpes discount 0.25 mcg calcitriol mastercard, the study was terminated for poor accrual, and ultimately fewer than 100 patients enrolled. The accrual goal for this trial was 660 patients, but it closed as a result of poor accrual enrolling a total of 278 patients (Sternberg et al. Because adjunctive radiation could substantially increase the risk for postoperative small bowel obstruction (Baumann et al. Despite the positive findings, the authors of the meta-analysis point out that insufficient evidence remains to base treatment decisions reliably. Notably, there were major deficiencies in the trials included in the meta-analysis such as small sample sizes, early closure of trials, limitations in statistical analysis, and differences in the way disease-free survival was defined (Sternberg and Collette, 2006). Despite the efforts of the trials outlined earlier, the evidence for adjuvant chemotherapy is lacking. An updated meta-analysis including 945 patients noted that adjuvant chemotherapy seems to be most beneficial to patients with node-positive disease; however, this metaanalysis was limited by many of the same issues outlined earlier (Leow et al. The available evidence suggests that perioperative chemotherapy does confer a survival benefit for bladder cancer patients with stronger evidence available in the neoadjuvant approach. The optimal approach and benefit to systemic chemotherapy in the adjuvant setting remains incompletely defined, and based on the difficulty with patient accrual in past trials it may remain unanswered. Bladder Preservation Although radical cystectomy remains the standard of care for patients with muscle-invasive bladder cancer, it is a major operative procedure with significant risk for perioperative morbidity and mortality (Shabsigh et al. Data from Medicare claims have shown radical cystectomy to have the second highest 30-day readmission rate compared with other urologic and nonurologic procedures (Goodney et al. The high incidence of perioperative complications, coupled with a classically older patient population with multiple medical comorbidities, has led patients and clinicians to seek alternatives to cystectomy. Bladder preservation is a curative intent paradigm that should be considered in two distinct populations: (1) patients who have high operative risks as a result of comorbidities and frailty and (2) patients who are fit for radical cystectomy but have limited burden of disease, adequate normal bladder urothelial and function, and are motivated to retain their bladder. Two basic strategies for trimodal bladder preservation exist: split-course and continuous-course therapy. Split-course therapy is based on the premise of mid-treatment restaging and is only appropriate for patients who are surgically fit and thus eligible for an immediate salvage cystectomy. In a split-course approach, patients are administered induction chemoradiation therapy to approximately 40 Gy, which is followed by restaging with cross-sectional imaging and endoscopic evaluation. Those without persistent invasive disease undergo consolidative chemoradiotherapy to approximately 60 to 64 Gy. As the name implies, continuous-course treatment involves a full course of chemoradiation therapy followed by an endoscopic restaging examination 3 to 4 months after therapy to allow time for an adequate response to therapy.
Jamguarandi (Jaborandi). Calcitriol.
- Diarrhea, eye problems, causing sweating, and other conditions.
- Dosing considerations for Jaborandi.
- Are there safety concerns?
- How does Jaborandi work?
- What is Jaborandi?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96285
Order 0.25 mcg calcitriol visa
In 1961 Francis and Jeffcoate reported a high incidence of dyspareunia after colporrhaphy with levator plication treatment arthritis buy calcitriol 0.25 mcg on-line. In addition, there is evidence to suggest that traditional posterior colporrhaphy with levator plication may worsen defecatory symptoms. Kahn and Stanton (1997) reported increased symptoms of fecal incontinence, constipation, incomplete evacuation, and dyspareunia postoperatively. Because of the increase in dyspareunia postoperatively, plication of the levator ani muscles has largely been abandoned. Site-specific repairs and midline fascial plication without levator ani plication have emerged as the predominant surgical treatments of a rectocele. Level 1 and Level 2 evidence support the superior objective outcomes of midline posterior plication without levatorplasty compared with site-specific repairs. However, if a patient requires an anterior or middle compartment repair, it should be performed first (Rovner and Ginsberg, 2001). The anterior wall can be retracted with a Heaney or Lone Star retractor with hooks to improve visualization. Hydrodissection may be accomplished by injecting saline or a local anesthetic with or without epinephrine. For a high rectocele the incision may be as high as the vaginal apex (cuff); for smaller rectoceles the incision is started at the most caudal position. The rectovaginal fascia (muscularis) is separated from the vaginal epithelium with Metzenbaum scissors. Native tissue sacrospinous hysteropexy with the posterior cervix attached to the right sacrospinous ligament and anterior colporrhaphy. The dissection proceeds laterally until the pararectal attachments to the pelvic sidewall are visualized. In cases of large posterior defects, a purse-string suture of 2-0 or 3-0 absorbable suture may be placed at the base of the rectal herniation to reduce it; however, care should be taken to avoid foreshortening the posterior wall cephalad to caudad. In addition, this acts to bring the attenuated rectovaginal fascia together to aid in its re-approximation. The rectovaginal fascia is then plicated in the midline with either interrupted or continuous 2-0 absorbable sutures. Care should be taken to avoid excessive lateral placement or wide spacing of these sutures; this may result in overtightening or painful ridges along the posterior vaginal wall. Suture placement is continued distally and incorporated into the perineal body re-approximation.
Effective 0.25 mcg calcitriol
This allows for assessment of distant and regional disease spread and can guide the use of neoadjuvant chemotherapy medicine video discount 0.25 mcg calcitriol mastercard. Although we do not advise on the routine use of oral antibiotic prophylaxis as an adjunct to mechanical bowel preparation, intravenous antibiotics should be administered within 1 hour of surgical incision. The choice of antibiotic should be customized to local bacterial susceptibility patterns and should include gram-positive coverage (skin flora) and gram-negative aerobes and anaerobes (distal small bowel and large bowel flora). Generally a broad-spectrum cephalosporin such as cefoxitin will provide adequate coverage. Last, in the absence of significant bleeding, high-risk patients should undergo both mechanical thromboembolic prophylaxis (pneumatic compression) and pharmacologic prophylaxis before the induction of general or spinal anesthesia. Extended prophylaxis in the postoperative period has also been shown to decrease thromboembolic events. A prospective study of 703 patients randomized to either 8 days or 28 days of pharmacologic prophylaxis after abdominal or pelvic surgery showed that those treated for 4 weeks had an 82. Patient positioning is vital to provide adequate exposure and to minimize the risk of related complications. Flexion to 15 degrees is usually adequate and can be lessened as necessary if there is a history of spinal fusion or lumbar injury. In women, a low lithotomy position with the aid of stirrups or the use of spreader bars provides access to the vagina. The operative field should be inclusive of the abdomen from the level of the xiphoid to the upper portion of the thighs. The genital organs, including the vagina in women, and the perineum should be prepared as well. A solution containing 10% povidoneiodine is recommended; preparations containing chlorhexidine gluconate should be avoided when used on genital skin. After confirmation before surgery of localized disease, patients should undergo routine medical evaluation to maximize health status. Comorbidities such as coronary artery disease, smoking-related lung disease, and peripheral vascular disease will commonly be encountered. After medical optimization, regardless of preferred urinary diversion, enterostomal therapy should be used for stoma marking. Although rare, patients should be made aware of the possibility of an ileal conduit urinary diversion even in the case of a planned continent diversion. Careful marking of the ostomy site to avoid interference, in a standing and in a seated position, is performed to maximize appliance fit and to minimize stomal irritation. If stomal therapists are not available, the surgeon should be familiar with marking strategies and should perform these while the patient is awake and wearing typical clothing. Mechanical bowel preparation was historically used in the hope of mitigated anastomotic leak, abdominal, and wound infections in patients undergoing bowel surgery.
Purchase calcitriol 0.25 mcg fast delivery
It is important to recognize that most urinary tract injuries do not result in a fistula symptoms of ms buy calcitriol 0.25 mcg low price. The relative proportions of the types of urinary fistula have changed with urethral fistulae having increased, whereas ureteral, bladder and/or urethral fistulae have decreased. At the Zekai Tahir Burak center in Turkey, 25,998 gynecologic and obstetric operations were performed over a 3-year period. If unrecognized intraoperatively, a pelvic urinoma may develop and ultimately drain out through the vaginal cuff. Tissue ischemia and then necrosis promote fibrosis and induration, finally resulting in an epithelial or mucosal lining of the tract and the development of a fistula tract. The degree of bladder injury appears to be a major factor in iatrogenic fistula formation. The bladder lacerations occurred during the hysterectomy portion of the surgery in 61% of cases and during the additional procedures in 39% (Mathevet et al. Most fistulae occurred as a consequence of caesarean section, surgical intervention, or hysterectomy for ruptured uterus (Raassen et al. The rate of urogenital fistulae associated with simple abdominal hysterectomy for benign disease is often described as being approximately 1 in 1000. In a national study from Sweden the rate of women undergoing any fistula surgery was reported as 0. From Finland the rate of vesicovaginal fistula was reported to be 1 in 1250 after all hysterectomies, 1 in 455 after laparoscopic, 1 in 1000 after total abdominal, and 1 in 5000 after vaginal hysterectomy (Harkki-Siren et al. The publicly available tables from the national hospital database in England give similar figures of 1 in 600 after total abdominal hysterectomy, and 1 in 5000 after vaginal hysterectomy (Herbert et al. More detailed longitudinal analysis of patientlevel information from the same data set suggests a rate of 1 in 788 for all types of hysterectomy, 1 in 540 for abdominal hysterectomy for benign disease, 1 in 896 after vaginal hysterectomy for benign disease (excluding prolapse), and 1 in 3861 after vaginal hysterectomy for prolapse (Hilton and Cromwell, 2012). Ketamine abuse can lead to not only severe changes in the bladder wall structure but also fistula formation, as was shown in 14. The operative approach to hysterectomy is an important factor, because bladder injuries are at least three times more common during abdominal hysterectomy compared with vaginal hysterectomy. Hilton calculated the risk for fistula formation in radical hysterectomy for cervical cancer to be 1 of 87, whereas in vaginal hysterectomy for prolapse, the risk was only 1 of 3861 (Hilton and Cromwell, 2012). It has been suggested that patients with severe abdominal pain, distention, paralytic ileus, hematuria, or symptoms of severe irritability of the bladder after abdominal hysterectomy be investigated early for a possible bladder injury (Kursh et al. Vaginoscopy has been suggested as an adjunct measure, in some cases, using a modified endoscope or flexible cystoscope to visualize precisely the fistula tract (Andreoni et al.
Calcitriol 0.25 mcg order online
A traction suture that has been placed on the ureter is then grasped with the hemostat symptoms 38 weeks pregnant purchase 0.25 mcg calcitriol mastercard, and the ureter is brought into the colon. Both ureters should be brought into the bowel before they are sutured to the mucosa. The technique originally described removal of a 2-mm button of seromuscular tissue. The seromuscular layer is incised, with care taken not to tent up the mucosa and inadvertently incise it. The holding suture in the ureter is grasped and drawn throughout the submucosal tunnel. The advantage of this anastomosis is that because the taeniae do not need to be aligned, one can form the tunnel according to the normal course of the ureter and avoid angulation. This technique reliably prevents reflux but results in a stricture rate of approximately 14% (see Table 139. After a distance of 3 to 4 cm has been achieved, a small hole is made in the serosa and the ureter is drawn through. Interrupted 5-0 polydioxanone sutures approximate the ureter to the full thickness of the mucosa and serosa. Although originally described for the small bowel, it may be used in any suitable intestinal segment. In the original description, the adventitia of the ureter was sutured with interrupted silk sutures to the serosa of the bowel. The mucosa and serosa were incised; a small mucosa plug was removed; and with fine absorbable chromic sutures, the full thickness of the ureter was sewn to the mucosa of the bowel. The anterior layer of ureteral adventitia was then sewn with interrupted silk sutures to the serosa of the bowel. A less cumbersome method of performing this anastomosis is to excise a small button of seromuscular tissue and mucosa, spatulate the ureter for 0. The ureters are drawn into the submucosal tunnel distally and sutured to the mucosa with 5-0 polydioxanone sutures proximally. Each suture includes the seromuscular layer of the taenia and the mucosa in the midline. The leakage rate is approximately 3%, the stricture rate is 6%, and the reflux rate isapproximately6%(seeTable139. The end of one ureter is sutured to the end of the other ureter, and this composite anastomosis is sutured to the end of the bowel. A head-to-tail ureteroureteral anastomosis is formed, which is then sutured to the end of the bowel. For the first anastomosis, a fine suture is placed at the apex of each ureter with the knot tied to the outside. They are performed in much the same way as a Bricker anastomosis would be performed for the small bowel (see later).
Purchase calcitriol 0.25 mcg mastercard
Hamid R symptoms thyroid problems order 0.25 mcg calcitriol overnight delivery, Bycroft J, Arya M, et al: Screening cystoscopy and biopsy in patients with neuropathic bladder and chronic suprapubic indwelling catheters: is it valid Ninkovic M, Stenzl A, Schwabegger A, et al: Free neurovascular transfer of latissimus dorsi muscle for the treatment of bladder acontractility.
Syndromes
- To develop ways of coping with the painful body sensations
- Spinal fracture
- Bone biopsy (rarely done)
- Getting lost on familiar routes
- Movement/coordination difficulties (apraxia)
- Worked with sheet metal in the past (you may need tests to check for metal pieces in your eyes)
- Serum potassium
- Have you been at a picnic, gathering, or similar event recently?
- Heart disease
Calcitriol 0.25 mcg purchase with amex
Although this trial did demonstrate an advantage in favor of adjuvant chemotherapy symptoms thyroid cancer buy calcitriol uk, it has been criticized for several reasons. This trial also highlighted the difficulty of administering chemotherapy after cystectomy with 25% of patients who were assigned to receive chemotherapy and who were not receiving therapy. Three-year disease-free survival was significantly improved in the chemotherapy arm (63% vs. This study was updated with a total of 83 patients (38 received chemotherapy after the close of the trial based on the interim analysis). Ten-year follow-up data maintained an advantage in the chemotherapy group with regard to progression-free survival (44% vs. Ultimately, 92% of patients in the observation arm showed evidence of tumor progression compared with 27% who received chemotherapy. Overall, the number of patients is small because of early closure of the trial after interim analysis. Many patients in the observation group were not offered chemotherapy at the time of disease progression and, as one would expect, not all patients randomized to chemotherapy ultimately received such therapy. Since the mid-2000s, there have been several attempts at large-scale adjuvant chemotherapy trials, most of which have been presented in abstract form. The chemotherapy cohort was randomly assigned to one of two regimens; either gemcitabine 1000 mg/m2 days 1, 8, and 15 and cisplatin 70 mg/m2 day 2 or the same gemcitabine schedule plus cisplatin 70 mg/m2 day 15, every 28 days. There was also no statistical difference in disease-free survival in the observation (42. The initial study was designed to randomize 610 patients in a 1: 1 fashion but was closed early because of poor accrual. The smaller sample size resulted in significant underpowering of the study in detecting a significant difference between adjuvant chemotherapy and observation. Continuous-course treatment is an appropriate option for both surgically fit and unfit patients. Given the same total dose, continuous-course treatment is more intensive than split-course treatment because continuous-course therapy is completed over a shorter period, which limits the opportunity for both tumor and normal tissue cell repopulation. Regardless of approach, the benefits of concurrent sensitizing chemotherapy during the course of radiation is now well-established. The rates of radical cystectomy for visibly complete resections are lower (11%) compared with incomplete resections (42%) (Efstathiou et al. Moreover, after pelvic failure is identified, outcomes are quickly catastrophic with a median survival of approximately 9 months (Baumann et al. There have been several clinical trials that evaluated the potential benefits of adjuvant radiation. A three-arm randomized trial performed at the National Cancer Institute in Cairo in the 1980s compared adjuvant radiation therapy alone (using two different radiation techniques) versus observation for patients with negative soft-tissue surgical margins but high risk for local failure following radical cystectomy alone (Zaghloul et al.
Order calcitriol 0.25 mcg amex
Renal mobilization and downward nephropexy may also be attempted as this can add up to 5 cm in ureteral length medicine nausea discount calcitriol 0.25 mcg overnight delivery. Lastly, reimplantation of the ureter into the bladder should avoid excessive angulation near its entry into the bladder as this may lead to postoperative obstruction. As a general rule, the ureter should be inserted into the bladder in a path directed toward the bladder neck. As alluded to earlier, the technique used for ureteral reimplantation depends in part on the clinical circumstances surrounding ureteral injury and the preference of the treating surgeon. Open surgery is preferred for trauma situations as this allows direct inspection of the abdomen and pelvis for associated injuries. Iatrogenic injury recognized intraoperatively may be managed using the same approach as the index procedure, although this depends on the comfort of the surgeon and the established surgical setup. The patient is placed on the operating table in the supine position with the anterior superior iliac spine positioned over the break of the table. The external genitalia and abdomen are sterilely prepped and draped to just above the level of the umbilicus. The subcutaneous tissue is divided with electrocautery down to the level of the rectus fascia. The rectus fascia is divided in the midline at the linea alba along the length of the incision. The underlying bellies of rectus abdominus muscles are subsequently split, permitting access to the transversalis fascia, which is divided the length of the incision to allow entry into the space of Retzius. The bladder is identified through palpation of the Foley catheter balloon, and the lateral pelvic gutters are developed with blunt dissection using a sponge stick, sweeping the perivesical fat medially. Adequate exposure of the great pelvic vessels will facilitate identification of the ureters. Alternatively, the ureter may be localized as it courses underneath the obliterated umbilical artery near its origin off of the proximal internal iliac artery. Using a right-angle clamp, the ureter is dissected circumferentially, allowing for placement of a vessel loop. Extravesical dissection of the ureter is then commenced caudad and cephalad taking care to avoid overskeletonization. In cases of ureteral stricture disease or iatrogenic injury, the diseased ureteral segment is identified and resected. A metal clip may also be placed across the ureter proximal to the diseased area as this will allow for passive ureteral distension and aid in subsequent reimplantation. Dissection within the lateral pelvic gutters is carried out superiorly, enabling cephalad displacement of peritoneal reflection off the bladder dome. The bladder should be disengaged from the overlying peritoneal reflection as much as possible using a gentle sweeping motion of the sponge stick in a cephalad-medial direction.
Order 0.25 mcg calcitriol mastercard
Pessaries should be removed and cleaned periodically treatment for hemorrhoids order calcitriol cheap online, and the tissue Continence Promotion and Advocacy Education of patients and providers is a critical aspect of continence promotion for older adults (Newman et al. In patients with limited hand dexterity or cognitive impairment, this may require assistance from a care provider. It is important that the pessary be routinely checked to avoid complications associated with neglect, including erosion into surrounding structures or vaginal infections. Concomitant use of vaginal estrogen can be useful to help prevent some of these complications. Pessaries offer potential advantages of avoiding surgery and allowing patients self-control over the clinical situation. Many older women do very well with pessaries and will continue to use them over time (Ramsay et al. Factors associated with increased long-term success include age of at least 72 years, careful fitting, and provision of clear instructions for use (Friedman et al. However, some older women do not like using pessaries or do not want to be bothered with having to remove and replace the device on a regular basis. If the pessary improves genitourinary symptoms but the patient does not like using the device, this may indicate that she could experience a good functional outcome with surgery. These procedures can be done using vaginal, laparoscopic, robotic, or open surgical techniques. A variety of native tissue repairs and procedures using biologic or mesh grafts can be used. However, as with any surgical treatment, patients do have to be very carefully counseled about use of mesh grafts and potential risks and benefits associated with this technique (Mohammed et al. However, in those who do eventually undergo surgical repair, there is evidence to suggest that increased time between development of symptoms, particularly after menopause, and subsequent surgery is associated with poorer subjective postoperative improvements (Ahn et al. In women who still have their uterus, the procedure is generally performed leaving lateral channels on each side of the vaginal vault to permit uterine drainage. Total colpocleisis is used in women after hysterectomy and consists of a denudation of the vaginal mucosa and subsequent reduction and conical closure of the prolapse. Perineoplasty is performed to reduce the size of the vaginal introitus and prevent recurrence of bulging from the outlet. Women must be expressly counseled that penetrative sexual activity will not be possible after this type of surgery. Reported success rates with colpocleisis have been high, and rates of subsequent regret after having the procedure are low (Koski et al. Colpocleisis has been shown to improve bladder and bowel symptoms in women with a history of significant prolapse (Gutman et al. Urethral caruncle is a protrusion of tissue from the urethra and is seen more commonly in elderly than in younger women. Unless they are large, they often do not affect voiding function (Ozkurkcugil et al.
Buy calcitriol without prescription
Clinical signs associated with common rheumatologic and neurologic disorders in older adults should also be evaluated professional english medicine buy cheap calcitriol. These include changes from arthritis and joint disorders, Parkinson disease, multiple sclerosis, prior stroke, spinal stenosis, cord compression, vertebral disc herniation, acute or chronic back pain, dementia, and delirium. Perineal sensation should be tested and may be diminished or asymmetric, particularly in those with a history of underlying neurologic disease. For example, patients with a history of stroke and associated hemiparesis may have asymmetric perineal sensation. Tissue quality should be assessed, including presence or lack of rugation of the vaginal mucosa. Atrophic vaginitis is common in postmenopausal women and is usually due to lack of estrogen. This can also lead to fusion or agglutination of the labia minora or labia majora. Vaginal narrowing or stenosis is another common finding on pelvic examination in elderly women. Many older women wish to void before pelvic examination because it makes this more comfortable, and they may be used to doing so before routine gynecologic examinations. In some cases, women want to void before examination to avoid potential embarrassment with urine leakage in front of the clinician. However, if the patient voids to completion before the examination, determination of stress leakage with cough or Valsalva will be severely limited. Gentle reassurance of the importance of doing the examination with urine in the bladder and objective identification of stress leakage can be very useful and can help put the patient at ease. Rectal examination may reveal signs associated with chronic constipation or fecal impaction. The bulbocavernosus reflex may be absent in older adults, although this change may or may not be associated with underling neurologic pathology. Prostate enlargement or nodularity may be palpable, although prostate size on rectal examination does not necessarily correlate with symptoms. Rectal cancers are more common among older adults, and the majority of lesions are palpable on digital rectal examination. Stool guaiac testing should also be considered and can help to identify otherwise silent pathology in some patients (Goetzl et al. Having the patient void as part of the physical examination can be particularly useful in geriatric patients. This may include actually taking the patients to the toilet to observe their behaviors and level of need for assistance.
Finley, 64 years: Bladder-sparing therapies with endoscopic resection and adjuvant chemotherapy and/or radiation have been examined (McPherson et al. Several hypotheses have been proposed for increased bladder cancer rates among men.
Leon, 32 years: Diagnosis Many studies exist for the diagnosis of enterovesical fistulae; however, there are significant problems with false negatives and false positives among the diagnostic modalities, and thus the diagnosis is often made on clinical grounds. One month later, the patient could void by contracting his rectus muscle, generating 50 cm H2O detrusor pressure.
Milten, 35 years: The typical history and clinical presentation of penile fracture usually make adjunctive imaging studies unnecessary. Deval B, Ferchaux J, Berry R, et al: Objective and subjective cure rates after trans-obturator tape (ObTape) treatment of female urinary incontinence, Eur Urol 49:373377, 2006.
Masil, 29 years: Certain patients may not be able to comprehend the strict flushing, irrigation, and catheterization regimens that must be followed after continent urinary diversion or may lack the motor skills to independently perform self-care. Reduced bladder capacity has been reported in several series (Thrasher and Crawford, 1992).
Brenton, 47 years: Indiana Pouch the concept of using the buttressed ileocecal valve as a dependable continence mechanism that can withstand the trauma of intermittent catheterization was first reported by Rowland et al. Patients with multiple sclerosis, quadriplegic individuals, and very frail or mentally impaired patients will at some point in their lives require family or visiting nurses for basic care and are therefore viewed as poor candidates for any form of continent diversion.
Esiel, 60 years: Lateral Space of Retzius and Anterior Vascular Pedicle Dissection After the sigmoid mesenteric release and the posterior dissection (male patients) attention is brought to the lateral dissection. The anastomosis was made using a submucosal tunnel in 809 renal-ureteric units and using a serosa-lined extramural tunnel in 74 units.
Jarock, 59 years: Sherif A, Rintala E, Mestad O, et al: Neoadjuvant cisplatin-methotrexate chemotherapy of invasive bladder cancer-Nordic cystectomy trial 2, Scand J Urol Nephrol 36(6):419425, 2002. For abdominal placement, a horizontal lower quadrant incision is made in the abdomen ipsilateral to pump placement.
Ateras, 61 years: Nevertheless, open surgery remains a widely utilized strategy with proven longstanding efficacy with respect to outcomes. Mucosal atrophy appears to be more reliable in small bowel than in large bowel reservoirs (Mills and Studer, 1999; Norlen and Trasti, 1978).
Arakos, 43 years: Thus cystoscopy and upper tract imaging are indicated in patients with hematuria and/or unexplained irritative symptoms (Davis et al. Patients should be counseled that surgical repair of the posterior compartment may likely reduce vaginal protrusion symptoms and decrease or eliminate the need for vaginal splinting.
Kadok, 63 years: Wei J, Dunn R, Marcovich R, et al: Prospective assessment of patient reported urinary continence after radical prostatectomy, J Urol 164:744748, 2000a. A barbed monofilament suture may facilitate suturing of the neobladder (Tyritzis et al.
Hurit, 54 years: Contraction is when the mesh exhibits "shrinkage or reduction in size," and prominence occurs when there are "parts that protrude beyond the surface. Studies with more frail and functionally impaired older adults may yield different results.
Lukjan, 38 years: Anal sphincteric tone must be judged competent before these operations are selected. In general, tissues less than 1 mm or more than 3 mm in thickness are not amenable to the use of staples.
Fedor, 34 years: In patients with intraperitoneal rupture, antimicrobial agents are administered for 3 days in the perioperative period only. Repeat urethral diverticulectomy surgery can be challenging because of altered anatomy, scarring, and the difficulty in identifying the proper anatomic planes.
Gnar, 48 years: Once disconnected from the bladder, the specimen is placed into a 10- or 15-cm EndoCatch bag. In a landmark population-based study of all incontinence procedures performed in Scotland from 1997 to 2016, mesh slings had fewer immediate complications and lower risk of future prolapse surgery than Burch colposuspension (Morling et al.
Hamid, 40 years: McCusker J, Cole M, Abrahamowicz M, et al: Delirium predicts 12-month mortality, Arch Intern Med 162:457463, 2002. Endovascular stenting is the preferred initial treatment, but open surgical interventions with urologic and vascular reconstructions may be necessary (Das et al.
Campa, 26 years: Sevestre S, Ciofu C, Deval B, et al: Results of the tension-free vaginal tape technique in the elderly, Eur Urol 44:128131, 2003. Overall rates of incontinence, anejaculation, and areflexic bladder are low (2% to 4%) (Anger et al.
9 of 10 - Review by Y. Umbrak
Votes: 166 votes
Total customer reviews: 166